You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Rosacea
Key points about rosacea
- Rosacea is a chronic inflammatory skin condition that mostly affects the skin on your face.
- Common symptoms are flushing, redness, and a lumpy rash, usually on your nose and cheeks.
- Rosacea can also cause eye problems. It's important to see your healthcare provider if you have eye symptoms.
- Symptoms can come and go and may be triggered by things such as too much sun exposure or stress.
- There's no cure for rosacea but treatments and self-care can help keep it under control.

Rosacea is a common, chronic (long-term) inflammatory skin condition that mostly affects your face (cheeks, nose, chin and forehead).
It mainly affects fair-skinned people, especially people of Celtic or Northern European origin, but may occur in any skin type. It affects about 5% of the world’s population. It can start in childhood, but most often appears between 30 and 60 years of age.
Rosacea isn’t contagious so you can’t pass it on to somebody else.
Symptoms include facial flushing, redness, acne-like spots, small visible blood vessels on your face, thickening of your skin, and eye problems such as dry eyes and sore eyelids.
Video: What is rosacea – patient explainers
(Patient, UK, 2018)
The cause of rosacea isn’t known for sure.
Possible contributing factors include:
- blood vessels changes under your skin
- sun damage
- a tiny mite called Demodex folliculorum, which is harmless in most people but can be present in higher numbers in people with rosacea
- inflammation due to abnormal immune reactions in the skin
- genetics (rosacea can run in families).
Certain things may trigger your rosacea and make it worse. These include:
- sunlight
- hot or cold temperatures
- wind
- emotional stress
- heavy exercise
- hot drinks
- spicy foods
- alcohol
- products that irritate your skin
- certain medicines, eg, topical corticosteroids such as hydrocortisone cream, or calcium channel blockers (used to treat heart conditions).
Rosacea is a chronic (long-term) condition, but your symptoms may come and go. You may get flare-ups, when your symptoms get worse, and periods when you have no symptoms.
The development and severity of rosacea symptoms can vary from one person to another.
Symptoms mainly affect your nose, cheeks, chin and forehead, although your neck, chest, ears and back can be affected – especially by flushing.
Rosacea isn’t usually painful or itchy, although you may have a tingling or burning feeling over your affected skin.
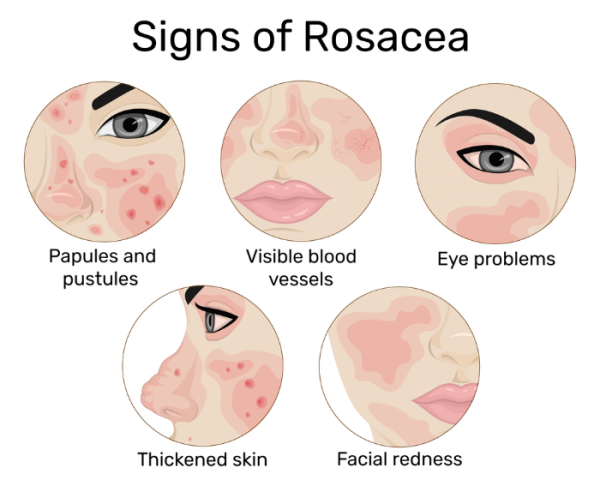
Image credit: Depositphotos
Symptoms of rosacea include:
- Flushing of your face (similar to blushing) due to vasodilation (widening of your blood vessels).
- Redness (erythema) of your face (similar to sunburn) – the reddened skin may turn rough and scaly.
- Small red bumps (papules) and cysts (pustules) that look like acne.
- Tiny visible blood vessels on your face (known as telangiectasia).
- Ocular rosacea, which may appear as sore, red, gritty, itchy, watery or dry eyes, sensitivity to light, or cysts, styes or inflammation of your eyelids.
- Thickening of your skin. You may develop an enlarged bulbous nose called a rhinophyma – this is uncommon, but more likely in men.
See a healthcare provider urgently if you develop eye pain or vision problems. These may mean you have a rare, but serious, complication affecting the front of your eye (the cornea), which may cause eye damage and vision loss if it isn’t treated.
Rosacea is usually diagnosed based on your symptoms and the appearance of your face. Specific tests aren’t usually needed.
Sometimes your doctor may do a blood test which can help tell if there is another reason for your skin redness, such as a condition called systemic lupus erythematosus.
There’s no cure for rosacea and there isn’t anything you can do to prevent it. However, there are effective treatments that can help reduce your symptoms, ease your discomfort and prevent rosacea from getting worse.
Before starting any treatment, you should make a note of any factors that trigger your rosacea and avoid these where possible. It’s a good idea to keep a diary(external link) to write down things that trigger your rosacea symptoms or make them worse.
Skincare advice
- It’s important to moisturise your skin regularly with a suitable moisturiser such as a non-greasy emollient. This helps to reduce moisture loss and improve skin texture, especially if your skin is dry.
- Use a gentle, non-soap cleanser.
- Limit the time you spend in the sun and apply sunscreen and wear a hat when you're outdoors.
- Don’t use creams and ointments that contain corticosteroid medicines (eg hydrocortisone cream) unless they've been recommended by your skin specialist (dermatologist) as they can make rosacea worse.
For flushing and redness
- Brimonidine gel (Mirvaso) can be used to reduce flushing and redness. It works by narrowing the blood vessels under the skin. Most people see their best results 3 to 6 hours after applying the gel. After that, redness will slowly return. Ask your healthcare provider how often you should use it. Long-term use can cause more flushing. It’s available on prescription but isn't funded so you will need to pay for it.
- If flushing is a big problem and brimonidine gel doesn’t help, your healthcare provider may prescribe, carvedilol or clonidine tablets. These medicines are not suitable for everyone and your healthcare provider will need to check your health and other medicines you're taking first.
- For persistent redness, light or laser therapy can be used to destroy tiny blood vessels under the skin without damaging nearby skin. This can treat telangiectasia (the small blood vessels you can see on your face) and improve redness. You can talk to your healthcare provider or skin specialist (dermatologist) about whether these treatments are suitable for you.
For acne breakouts and cysts (papulopustular rosacea)
- For mild breakouts, creams or lotions can be used to treat a few spots. Examples include azelaic acid cream or lotion (Skinoren, Acnederm, Azclear), metronidazole cream or gel or ivermectin cream but it's an unapproved medicine and not funded in Aotearoa New Zealand.
- For moderate breakouts, antibiotics such as doxycycline tablets or erythromycin capsules may be used to reduce inflammation. These antibiotics are effective because of their anti-inflammatory effect. It can take 6 to 12 weeks to clear spots and cysts, and you might need more courses of treatment if they return. Some people take this longer term to prevent spots and cysts from coming back.
- For severe acne, isotretinoin tablets may be prescribed when other treatments are not helping.
For ocular rosacea (eye problems)
- It’s important to see your healthcare provider if you develop eye problems. They may refer you to an eye specialist (ophthalmologist).
- Use artificial tears for lubrication if you have dry eyes.
- Practice good eyelid hygiene if you have inflammation of the eyelids (blepharitis). Read more about blepharitis and eyelid hygiene.
- Your doctor may recommend antibiotics, such as those used for rosacea spots and cysts (see above), if your eye symptoms bother you.
- An ophthalmologist may prescribe corticosteroid eyedrops if you develop inflammation of the front of your eye (the cornea).
For rosacea of your nose (rhinophyma):
Rhinophyma (an enlarged bulbous nose) is an uncommon symptom of rosacea. It’s more common in men than in women.
- Doxycycline and isotretinoin tablets can stop rhinophyma from getting worse.
- Surgery or laser treatment may be used to trim the thickened skin on your nose and improve its appearance.
There are many things you can do to help manage your rosacea.
- Avoid sunlight – wear a hat and use a high protection factor, oil-free facial sunblock every day on your face and re-apply it often when you’re outside. A suitable sunblock is one with SPF 30 or higher with ultraviolet A and B protection. You may find that you tolerate a physical sunscreen (zinc oxide/titanium oxide) better than a chemical one. Read more about sun safety.
- Avoid other possible triggers that make your rosacea worse, such as:
- extreme heat or cold
- wind
- alcohol
- strenuous exercise
- stressful situations
- sunlight
- spicy food
- hot drinks
- hot baths or showers.
- Avoid corticosteroid creams or other abrasive creams on your face.
- Use a soap substitute (emollient) to wash your face.
- You may prefer to use an electric razor rather than a blade when you shave.
- If you have dry skin, try a hypoallergenic, non-perfumed, non-greasy moisturising cream.
- Try holding some ice in your mouth for a short time between your gum and cheek to temporarily reduce redness.
- Avoid products that may make your skin more sensitive, eg, cleansers that contain acetone or alcohol, abrasive or exfoliant products, oil-based or waterproof make-up, perfumed sun blocks.
- Cosmetics with green or yellow tint may help conceal redness on your face.
- Eat a healthy diet. Read more about healthy eating.
- Be alert for eye symptoms. See your healthcare provider or eye specialist (ophthalmologist) if your eyes become affected.
- Practice good eyelid hygiene and avoid wearing contact lenses if you have eyelid inflammation (blepharitis).
- Some medicines, eg, calcium channel blockers (which are used to treat various heart conditions) may trigger flushing and make it worse. Your healthcare provider may be able to prescribe a different medicine.
Rosacea isn’t life-threatening, but it is a chronic (long-term) condition. Your symptoms may come and go and you’ll need ongoing treatment if you have flare-ups.
You may have only have minor cosmetic changes or you may have severe damage to the skin on your face. Rosacea can generally be controlled with treatment, but some people keep having relapses or find that their condition continues to progress.
If your symptoms are well controlled, this can increase the time between relapses and help to improve your quality of life.
The rash and flushing you experience with rosacea can lead to embarrassment, lowered self-esteem and self-confidence, anxiety and depression. Many people with rosacea say that it affects their personal and social lives.
Contact your healthcare provider if your rosacea is causing emotional problems. They can refer you for psychological support or there are in-person or online support groups that you can join (not specifically for rosacea within Aotearoa New Zealand).
Coping with rosacea – lifestyle management for rosacea patients(external link) National Rosacea Society, US
Rosacea diary – an easy way to find and avoid your personal rosacea triggers(external link) National Rosacea Society, US
References
- Rosacea(external link) DermNet, NZ, 2022
- Rosacea(external link) British Association of Dermatologists, UK, 2022
- Rosacea(external link) Patient, UK, 2023
- Rosacea basics(external link) National Institute of Arthritis and Musculoskeletal and Skin Diseases, US, 2024
British Association of Dermatologists guidelines for the management of people with rosacea 2021(external link), British Journal of Dermatology, UK, 2021
Rosacea – seeing red in primary care(external link) BPAC, NZ, 2016
Rosacea(external link) Australian Family Physician, Australia, 2017
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor; Angela Lambie, Pharmacist, Auckland
Last reviewed:





