A migraine attack can have distinct phases.
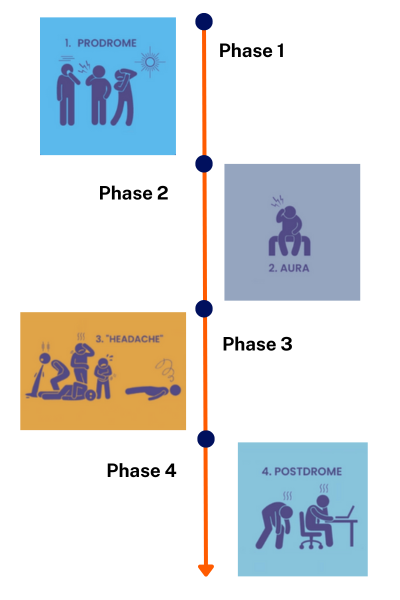
Image credit: Adapted from Migraine Foundation, NZ with permission
Phase 1 – prodome
Some people can feel early warning signs that tell them a migraine attack might be coming soon. These warning signs, that can occur a few hours to a few days before the headache starts, are called prodromal symptoms. About 8 in 10 people get prodromal symptoms.
Examples of prodromal symptoms include:
- feeling tired, fatigue
- repeated yawning
- restlessness or irritability
- anxiety
- food cravings, feeling hungry or thirsty
- difficulty concentrating
- dizziness
- sensitivity to light or sound
- neck pain.
Phase 2 – aura
Just before the headache starts you may have changes in 1 or more of your senses of sight, smell, hearing and touch. These changes are part of the "aura" phase. Only about 1 in 4 people with migraine experience aura, so if you've never had these symptoms it doesn't mean you don't have migraine.
Examples of aura symptoms are:
- problems with vision (seeing zig-zag lines, flashing lights or spots in your vision)
- hearing loss or a ringing sound in your ears
- feelings of tingling or numbness in your body.
Phase 3 – headache
When the headache starts, it's a strong pain, usually on one side of your head. You may feel sick or vomit (be sick), get tingling around your mouth, have trouble talking or feel dizzy or weak.
Phase 4 – Postdrome
The final phase of a migraine attack is the postdromal (or 'hangover') phase. This is when your headache has resolved but other symptoms (eg, fatigue, nausea and difficulty thinking) continue for a day or more.
Read more about the phases of a migraine attack(external link).