You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Fingolimod
Sounds like ' finn-GOLLY-mod'
Key points about fingolimod
- Fingolimod is used to treat multiple sclerosis.
- Fingolimod is also called Gilenya.
- Find out how to take it safely and the possible side effects.

Fingolimod is used to treat relapsing remitting multiple sclerosis (MS). This type of MS involves recurrent acute episodes (relapses), with symptoms suddenly increasing or new symptoms developing. This is followed by periods when symptoms improve or even disappear altogether (remissions). Fingolimod belongs to a group of medicines called disease-modifying therapies which help to slow or reduce the worsening of disability in people with relapsing remitting MS.
Fingolimod acts on certain types of white blood cells called lymphocytes.
- In MS, these small lymphocyte cells play a role in destroying myelin, the protective sheath that surrounds the nerve fibres and helps with the efficient flow of nerve signals or messages to and from the brain and various parts of the body.
- Fingolimod helps prevent lymphocytes leaving the lymph nodes.
- This lowers the number of lymphocytes circulating in the blood and reaching the central nervous system, which in turn reduces damage to the nerve cells in the brain and spinal cord.
-
Read more about multiple sclerosis.
In Aotearoa New Zealand fingolimod comes as capsules (500 micrograms).
- Always take fingolimod exactly as your doctor has told you. The pharmacy label will tell you how much to take, how often to take it and any special instructions.
- The usual adult dose is 1 capsule once a day.
- Note: The first dose of fingolimod is given in a doctor's clinic, where you will be observed for 6 hours to monitor your heart rate. After this first dose, you can take the remaining doses at home.
- If you stop taking fingolimod for more than 2 weeks and then restart, you'll need to follow the same process when having your first dose. Read more in the section on what you need to know before starting fingolimod, below.
- Swallow the capsule whole with a glass of water.
- You can take fingolimod with or without food.
- Take your dose at about the same time each day.
- If you forget to take your dose, take it as soon as you remember. But if it's nearly time for your next dose, take the next dose at the right time. Don't take extra doses to make up for a forgotten dose.
- If you've missed a dose on 1 day during the first 2 weeks, contact your doctor right away.
Tests to monitor your heart rate
Fingolimod can cause your heart rate to slow down, especially after you take the first dose, so you'll need to be carefully monitored.
- You'll have an electrocardiogram (ECG) at a medical clinic, to check the electrical activity of your heart before you take your first dose. You'ill be observed for at least 6 hours after your first dose.
- If your heart rate slows down too much during this time, you may notice dizziness, tiredness, feeling like your heart is beating slowly or skipping beats or chest pain.
- These symptoms of slow heart rate will usually happen during the first 6 hours after your first dose.
- If you develop these symptoms, you will need to have another ECG. If your ECG shows any heart problems or if your heart rate is still too low or decreases further, you will continue to be observed.
- If you have any serious side effects after your first dose, you'll need to stay in the medical clinic overnight.
- You will also be observed for at least 6 hours after you take your second dose the next day.
- If you have certain types of heart problems, or you're taking a type of medicine that can affect your heart, you'll be observed overnight after you take your first dose.
- If you stop taking fingolimod for more than 2 weeks and it is later re-started, you will need to follow the same process as having your first dose.
Tests to monitor your eyesight
Fingolimod can cause a problem with your vision called macular edema. Macular edema can cause some of the same vision symptoms as a multiple sclerosis (MS) attack (optic neuritis). Some people may not notice any symptoms with macular edema. If macular edema happens, it usually starts in the first 3 to 4 months after you start taking fingolimod.
- Your doctor will test your vision before you start fingolimod and 3 to 4 months afterwards.
- Your risk of macular edema is higher if you have diabetes or have had an inflammation of your eye called uveitis.
- Call your doctor right away if you have any of the following:
- blurriness or shadows in the centre of your vision
- a blind spot in the centre of your vision
- sensitivity to light
- unusually coloured (tinted) vision.
Here are some things to know when you're taking fingolimod. Other things may be important as well, so ask your healthcare provider what you should know about.
- Increased risk of infections: Fingolimod weakens your body’s defence (immune) system, so you're more likely to pick up infections. It's important to avoid anyone who has chickenpox or shingles. Check with your doctor if you need to have vaccinations for these before you start taking fingolimod.
- Skin checks: Contact your doctor if you notice any changes to your skin such as moles, freckles, or skin nodules, and sores that don't heal.
- Pregnancy: You should avoid becoming pregnant while you're taking fingolimod and for at least 2 months after you stop treatment. Talk to your healthcare provider about contraception options for you and your partner. Tell your healthcare provider if you become pregnant while taking fingolimod.
- Vaccines: Some vaccines shouldn't be taken after you've started taking fingolimod. Always check with your doctor or pharmacist first. It's safe for you to have the annual flu vaccine.
- Other medicines: Fingolimod may interact with a few medicines and herbal supplements, so check with your doctor or pharmacist before starting fingolimod or before starting any new medicines, including those you can buy over-the-counter.
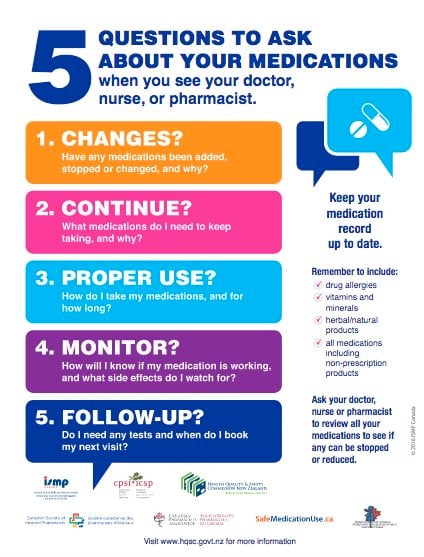
Like all medicines, fingolimod can cause side effects, although not everyone gets them. Often side effects improve as your body adjusts to the new medicine. You will need to have regular blood tests to check for some side effects while you're taking fingolimod, especially during the first year of treatment. You will also need regular eye tests and a skin check every year.
| Side effects | What should I do? |
|---|---|
|
|
|
|
|
|
|
|
|
|
| Read more about medicines and side effects and reporting a reaction you think might be a side effect. | |
The following links provide further information about fingolimod. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
- Gilenya(external link) Medsafe consumer medicine information, NZ
- Gilenya (Fingolimod)(external link) Multiple Sclerosis New Zealand
- Fingolimod (Gilenya)(external link) MS Society, UK
References
- Fingolimod(external link) New Zealand Formulary
- Gilenya(external link) Medication Guide, Novartis
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:





