If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Copaxone
Also called glatiramer acetate
Key points about Copaxone
- Copaxone is used to treat multiple sclerosis.
- Copaxone is also called glatiramer acetate.
- Find out how it's given and the possible side effects.

Copaxone is used to treat relapsing remitting multiple sclerosis (MS). Copaxone belongs to a group of medicines called disease-modifying therapies which help to slow or reduce the worsening of disability in people with relapsing remitting MS.
- MS is caused by your immune system mistakenly attacking the myelin sheath in your brain and spinal cord.
- It's thought that specific types of B cells and T cells in your body are involved in the attack.
- It's not fully understood how Copaxone works – it's thought to act by altering immune processes that cause MS.
Read more about multiple sclerosis.
In Aotearoa New Zealand, Copaxone is available as a prefilled syringe for injection, which is ready for use. It's given by a subcutaneous injection into the fatty layer under the skin. Each syringe is 40 mg.
- Always use Copaxone exactly as your doctor has told you. The pharmacy label will tell you how much to take, how often to take it, and any special instructions.
- The usual dose is 20 mg injected once daily or 40 mg three times a week (at least 48 hours apart, eg, every Monday, Wednesday and Friday).
Copaxone is given as an injection under your skin (subcutaneous injection). Some people can give themselves the injection or it can be given by another person. This could be a family/whānau member or friend after proper training, or your healthcare provider.
Preparation
Copaxone is usually stored in the fridge. Take your syringe out of the fridge and leave it at room temperature for 20 minutes before injecting. Don't warm Copaxone in any other way, eg, in the microwave or in hot water. Syringes may be stored out of the fridge for up to 30 days. If you take them out of the fridge, write the date on the pack and use them within 30 days.
Injection sites
Each injection should be given at a different site. Choose an injection site, such as on the front of your thighs or your abdomen (belly) at least 5cm from your belly button. A caregiver may also give you an injection in your upper arm. The injection site should be different from your last injection site. Don't inject into skin that is sore, bruised, red, hard or scarred or that has stretch marks.
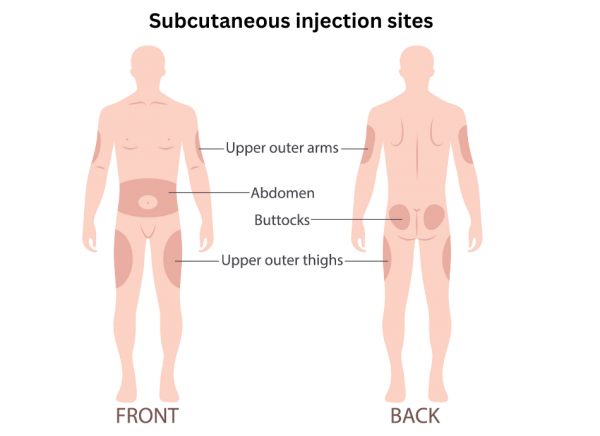
Image credit: Depositphotos
Here are some things to know when you're taking Copaxone. Other things may be important as well, so ask your healthcare provider what you should know about.
- Increased risk of infections: Copaxone weakens your body’s defence (immune) system, so you're more likely to pick up infections. It's important to avoid anyone who has chickenpox or shingles.
- Vaccines: Some vaccines shouldn't be given if you are taking Copaxone. Always check with your doctor or pharmacist first. It's safe for you to have the annual flu vaccine.
- Other medicines: Copaxone may interact with a few medicines and herbal supplements, so check with your doctor or pharmacist before starting Copaxone or before starting any new medicines, including those you may buy over-the-counter.
Like all medicines, Copaxone can cause side effects, although not everyone gets them. Often side effects improve as your body adjusts to the new medicine.
| Side effects | What should I do? |
|---|---|
|
|
|
|
|
|
|
|
|
|
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
The following links provide further information about Copaxone. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Copaxone(external link) Medsafe consumer medicine information, NZ
Copaxone(external link) Multiple Sclerosis New Zealand
Glatiramer acetate (Copaxone and Brabio)(external link) MS Society, UK
References
- Glatiramer acetate(external link) New Zealand Formulary
Brochures

Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:





