Insulin pumps
Key points about insulin pumps
- An insulin pump is a small device used by people with diabetes (mate huka), that can be used to deliver insulin to match your body’s needs.
- It's designed to copy how your pancreas would naturally release insulin.
- Insulin pump users deliver almost all of their insulin through their pump.
- From 1 October 2024 Pharmac has made it easier to access insulin pumps in people who meet their criteria and have been assessed by a specialist diabetes services.

Overview
An insulin pump is a small battery-operated device, used by people mainly with type 1 diabetes. It's a similar size to a small mobile phone and can be clipped to your belt or waistband, carried in your pocket or in a pouch.
- Insulin pumps consist of the pump itself, a disposable reservoir to store the insulin, and a disposable infusion set.
- The infusion set includes the tubing that connects the pump to a smaller fine tube (or cannula) which sits just under your skin. Read more about how an insulin pump works.
- An insulin pump continuously releases small amounts of rapid acting insulin to keep your blood glucose levels steady between meals and during sleep. (This replaces the long-acting insulin that most people inject once a day).
- The pump is also used to release insulin to your body when needed, such as during a meal or snack, to help manage your glucose levels.
Using an insulin pump can improve blood glucose management and reduce the number of severe hypoglycaemic events for people with type 1 diabetes compared to multiple daily injections.
It's important to remember that you must continue to check glucose levels using a continuous glucose monitor (CGM) or glucose meter.
From 1 October 2024 Pharmac has made it easier to access insulin pumps in people who meet their criteria and have been assessed by a specialist diabetes services.
There are 2 insulin pumps which are funded – mylife YpsoPump and Tandem t:slim pump. Read more below about which pumps are funded in Aotearoa New Zealand(external link).
You can also find information about diabetes technology on KidsHealth(external link).
Insulin pumps consist of the pump itself, a disposable reservoir to store the insulin, and a disposable infusion set. The infusion set includes the tubing that connects the pump to a fine tube (or cannula) which sits just under your skin.
An automated insulin delivery system (AID) is when the pump is used together with a CGM plus an algorithm, that links the 2 devices together, enabling them to “talk” to each other. In this way, the pump can receive blood glucose readings from a CGM and calculate how much insulin to deliver based on your current and predicted glucose values. Read more about automated insulin delivery (AID) system.
How is the insulin pump connected to my body?
The pump is connected to your body through an infusion set, so the insulin can be delivered.
- The infusion set is a thin plastic tube that’s connected to a fine tube (or cannula) which sits just under your skin.
- The tube is inserted where you would give insulin injections, and is designed to be pain free.
- The tube needs to be changed every 3 days.
- You can remove the tubing when you have a bath, go swimming, or when you play sports.
- The plastic tube is also called 'insulin pump consumables'.
How is insulin delivered through the pump?
The insulin pump holds insulin. An insulin pump is designed to copy how your pancreas would naturally release insulin. Insulin pump users deliver almost all of their insulin through their pump.
- The pump is programmed to give insulin at a continuous low rate during the day and night. This is called background insulin or basal insulin.
-
It's also used to give additional insulin at mealtimes, by entering the number of grams of carbohydrate you've eaten into the pump. The pump then delivers extra insulin for meals – this is called bolus insulin. The insulin pump will also deliver extra insulin if glucose levels are too high. These are known as corrections.
An automated insulin delivery system is made up of an insulin pump plus a continuous glucose monitor (CGM) plus an algorithm that links the 2 devices together, enabling them to “talk” to each other.
- An AID is like a standard insulin pump with one major difference – they have algorithms that can receive blood glucose readings from a CGM and calculate how much basal insulin to deliver based on your current and predicted glucose values.
- When a bolus dose is needed for a meal and/or correction, these systems also have calculators that can suggest a bolus amount.
- Bolus delivery is not automatic, manual programming and delivery is needed just like a standard insulin pump.
The automatic adjustments help to keep your glucose in the target range. You would still need to prompt the pump to deliver bolus doses for meals and adjust for exercise.
In New Zealand, AIDs are now funded for people who meet specific criteria, and have had an assessment by a specialist diabetes services.
In Aotearoa New Zealand you are eligible to get a funded insulin pump if you have:
- type 1 diabetes
- permanent neonatal diabetes (diabetes since you were born)
- some types of “monogenic diabetes” with insulin deficiency
- type 3c diabetes, which includes insulin deficiency caused by pancreatectomy, cystic fibrosis related diabetes or pancreatitis
- some atypical inherited forms of diabetes.
AND your diabetes specialist team agree:
- an insulin pump is right for you, and
- you will benefit from an automated insulin delivery (AID) system.
A specialist diabetes service includes many health professionals who are trained to assist people living with diabetes. Your primary healthcare provider may be able to refer you to them.
Learn more about who can get an insulin pump.(external link)
There are 2 insulin pumps which are funded – mylife YpsoPump and Tandem t:slim pump. Both pumps are compatible with at least 2 types of continuous glucose monitor (CGM). If you qualify for a funded insulin pump, you can also get funded CGMs. Read more about CGMs.
Note: The Tandem t:slim X2 will also work with the FreeStyle Libre 3 by July 2025.
Each pump's algorithm works differently, so your diabetes specialist team will discuss with you, which is the best option for you. For the differences between the pumps, see:
- Compare insulin pumps with AID(external link) (Aotearoa Diabetes Collective)
- Pump comparison sheet(external link) (Diabetes NZ)
- Compare funded insulin pumps(external link) (Pharmac)
mylife YpsoPump
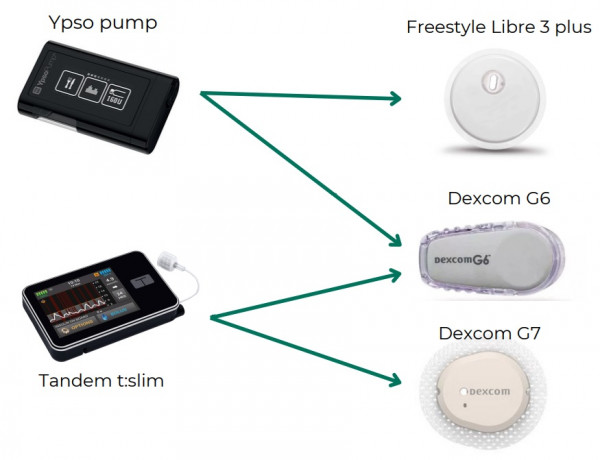
- The mylife YpsoPump works with either the Freestyle Libre 3 plus CGM or Dexcom G6 CGM.
- It uses the mylife CamAPS FX automated insulin delivery system software (algorithm), to calculate the dose of insulin to administer directly into your body.
- Read more about the mylife YpsoPump(external link).
- Also see Back-up kit checklist YpsoPump(external link) (Aotearoa Diabetes Collective).
Tandem t:slim pump
- The Tandem t: slim pump works with either the Dexcom G6 or Dexcom 7 CGMs.
- It uses the Basal-IQ or Control-IQ automated insulin delivery system (algorithm) software to calculate the dose of insulin to administer directly into your body.
- Read more about the Tandem t:slim pump(external link).
- Also see Back-up kit checklist for Tandem t:slim X2(external link) (Aotearoa Diabetes Collective).
Medtronic MiniMed 770G insulin pump will be discontinued
From 1 January 2025 the Medtronic MiniMed 770G insulin pump will no longer be funded for people new to insulin pumps. From 1 October 2026 the consumables for the MiniMed 770G insulin pump will no longer be funded. Read more about Medtronic (MiniMed 770G) insulin pumps – what's changing(external link).
Your diabetes specialist team will offer you the training and support you need to get the most from an insulin pump and CGM.
The suppliers of the insulin pumps are offering phone support from 1st October 2024.
- Tandem t:slim x2 (supplier: NZMS): 0508 634 103
- mylife YpsoPump (supplier: Pharmaco): 0800 458 267
Problems with the insulin pumps and CGMs
- Faulty insulin pumps: If the insulin pump is faulty, or an issue develops, you will need to contact the supplier.
- Faulty CGMs: If you're having trouble with your CGM or think it may be faulty, contact the supplier or your pharmacy for help. If it's faulty, the suppliers will provide you a replacement free of charge. Any CGMs provided to replace faulty ones would not count towards your annual limit.
- Broken or lost insulin pumps: If your insulin pump is broken or lost, talk to the supplier about your options. But be aware that you may need to pay for a replacement. Pharmac funds 1 new insulin pump every 4 years which is the warranty period on insulin pumps. You may be able to claim a broken or lost insulin pump on your household insurance.
- Broken or lost CGMs: There's a limit on the total number of CGMs you can have each year that takes this into account. If you’ve used more than the limit, you may need to pay for more CGMs. Check how many CGMs you can get.
Always be prepared
- Ask your healthcare provider about an action plan so you know what to do if your insulin pump stops working. If this happens, contact the helpline of the insulin pump supplier for a replacement and let your diabetes nurse specialist know. You should get a back-up pump within 24h. In the meantime, give yourself insulin using an insulin pen within 4 hours of the pump stopping guided by your pump records.
-
Ensure you have enough insulin for emergencies. As part of your emergency planning, you should have any medication or equipment supply for at least three days. The Tandem t:slim X2 insulin pump has a rechargeable battery, which needs power to re-charge. The mylife YpsoPump uses AAA batteries. It's a good idea to keep spare batteries and some charging packs for your phone and your pump in your grab bag and make sure you also have spare consumables.
Travelling with diabetes
- Diabetes and travelling(external link) Diabetes New Zealand
- Navigating airport security screening: Guidance for people living with diabetes(external link) Aviation Security Service, NZ
- Travelling with children who have diabetes(external link) KidsHealth NZ
- Travel(external link) Diabetes Australia
- Travel and type 1 diabetes(external link) Diabetes Australia
Disposing of your insulin pump
Insulin pumps consist of the pump itself, a disposable reservoir to store the insulin, and a disposable infusion set. The insulin pump insertion needle (not the tubing) must be disposed of in a sharps bin. Read more about the safe disposal of syringes, needles and other sharps.
Funding announced for continuous glucose monitors (CGMs) and insulin pumps(external link) Diabetes New Zealand
Continuous glucose monitors (CGMs) and insulin pumps(external link) Pharmac, NZ
mylife YpsoPump(external link)
Tandem t:slim pump(external link)
Diabetes technology(external link) KidsHealth, NZ
Brochures
Navigating airport security screening(external link) Aviation Security Service New Zealand and Diabetes New Zealand
Insulin Pumps with diabetes [PDF, 2.4 MB] Lilly Diabetes, Royal College of Nursing, UK
Apps
References
- Insulin pumps(external link) Diabetes New Zealand, NZ, 2024
- Funding announced for continuous glucose monitors (CGMs) and insulin pumps(external link) Diabetes New Zealand, NZ, 2024
- Glucose monitoring in children with diabetes(external link) KidsHealth, NZ, 2022
- Blood sugar levels can fluctuate for many reasons(external link) Mayo Clinic, US, 2022
Brochures

Which CGMs work with which insulin pump?
PHARMAC, NZ, 2024

Navigating airport security screening Aviation Security Service New Zealand and Diabetes New Zealand
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Claire Salter, Clinical Pharmacist, Tauranga; Angela Lambie, Pharmacist, Auckland
Last reviewed:






