You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Continuous glucose monitors
Also known as CGMs
Key points about continuous glucose monitors
- A continuous glucose monitor (CGM) is a device used by people with diabetes (mate huka) to measure glucose levels every few minutes without the need for finger pricking.
- A CGM is useful for showing patterns in your glucose levels and alerting you if your blood glucose is getting too low.
- CGMs can be used by themselves (standalone) or with a compatible insulin pump.
- In Aotearoa New Zealand some types of CGMs are funded by Pharmac for people who meet their criteria.

A continuous glucose monitor (CGM) is a small device people with diabetes can wear that measures their glucose levels every few minutes throughout the day and night. The readings are sent to a receiver which can be programmed to sound alarms and send alerts if your glucose levels are outside your set target range – if they're getting too high or too low. The information can also be used to produce reports which show trends and patterns in your glucose levels to help you get better diabetes control. Read more about how a CGM works.
What are the benefits of CGMs?
The aim of diabetes management is to keep your glucose levels in a healthy range. To do this well you need to monitor your glucose levels regularly. You can do this with finger-prick tests and a blood glucose monitor. This gives you a snapshot of your glucose levels at the time of the test. Because CGMs continuously track your glucose levels, including telling you whether the level is rising or falling, people who use a CGM often have better blood glucose management compared to those using finger-prick testing.
- You can see trends and patterns in your glucose levels for better diabetes management: The information collected from the CGM will show you what your glucose level is right now and will put all your readings together into a graph. This lets you see how much time your blood glucose level stays within range each day, and records times when it goes too high or too low. This shows a full picture of how your glucose levels change over time and how food and drink, physical activity, stress, and being sick change your results.
- You can notice and respond to changing glucose levels quickly: Most CGMs can send you or your caregiver an alert when your glucose levels get too high or low. This makes it much easier to act before there is a problem.
Finger prick tests are still important
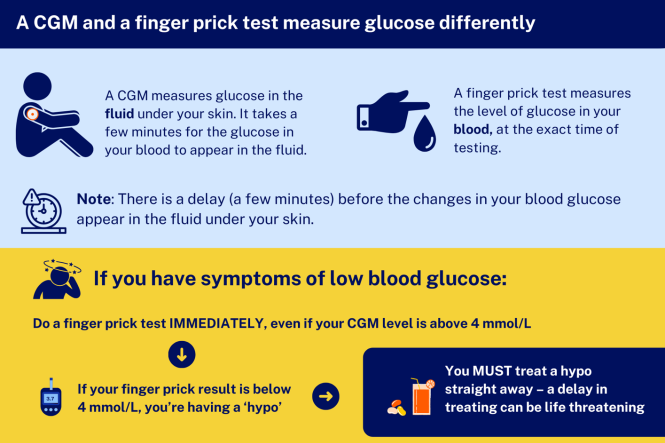
Image credit: Healthify He Puna Waiora
For more information see the section below on can I stop doing finger prick checks to monitor my blood glucose if I have a CGM?
Funding of CGMs for people in Aotearoa New Zealand
- Find out who can get funded CGMs below.
- CGMs can be used by themselves (called standalone CGMs) or may be used with a compatible insulin pump.
- CGMs are currently not funded for people with type 2 diabetes. Read more about why type 2 diabetes isn't included(external link).
You can also read about diabetes technology(external link) and glucose monitoring for children with diabetes(external link) on the KidsHealth New Zealand site.
A continuous glucose monitor(CGM) has 2 main parts:
- The sensor which is a small device that sits on your skin. It contains a fine probe, which measures glucose levels in the tissue just under your skin, and a transmitter, which sends the glucose readings to a receiver. The sensor is disposable and needs to be changed every 10 to 14 days (depending on the brand). Some CGMs come with an applicator to make it easier to attach the sensor.
- The receiver displays the glucose results. A receiver can be a reader, a smartphone app or an insulin pump. The sensor manufacturer can supply you with a free reader if you need one.
The CGM measures the glucose in the fluid surrounding your cells (interstitial fluid) every few minutes, 24 hours a day. This can easily show patterns and trends in your glucose levels.
You can set alarms for high and low glucose levels. However, if your symptoms don't match the CGM readings it's important to double check your glucose levels by using finger-prick tests.
Glucose levels that go up and down a lot can be damaging for your body. Very high (hyperglycaemia) or low blood glucose levels (hypoglycaemia) can be serious.
In Aotearoa New Zealand, Pharmac funds CGMs, insulin pumps and insulin pump equipment (consumables) for people with:
- type 1 diabetes
- permanent neonatal diabetes (diabetes since you were born)
- some types of monogenic diabetes with insulin deficiency
- type 3c diabetes which includes insulin deficiency caused by pancreatectomy, cystic fibrosis-related diabetes or pancreatitis
- some atypical inherited forms of diabetes.
If you’re not sure whether this includes your type of diabetes, your doctor or diabetes specialist team will be able to help.
How can I get a funded CGM?
You will need to make an appointment with your doctor or a member of your diabetes specialist team. They will apply for funding through a Special Authority. In most cases you can get a Special Authority on the same day, but sometimes this can take a bit longer.
- Once you have a Special Authority, your GP or diabetes specialist team can write prescriptions for CGMs. Your first Special Authority is valid for one year. You will need a new prescription every 3 months.
- Prescriptions are filled at your usual pharmacy in the same way as your other medicines. If you don't qualify for free prescriptions, you may need to pay a co-payment (usually $5) at the pharmacy.
- Every year, your doctor or your specialist diabetes team will check if you’re still getting benefit from the devices and apply for a new Special Authority.
Read more about the funding of the following by Pharmac:
- What's funded for who?(external link)
- Continuous glucose monitors(external link)
- Insulin pumps and consumables(external link)
Can I get a funded CGM if I have type 2 diabetes?
No, CGMs for people with type 2 diabetes are not currently funded by Pharmac but they acknowledge there is emerging evidence for these to help people with type 2 diabetes. Read more about why type 2 diabetes isn't included.(external link)
Note: A new, more affordable CGM is now available in New Zealand for people with type 2 diabetes. The CareSens Air CGM costs significantly less than other CGMs currently on the market. Learn more about the CareSens Air CGM(external link).
A standalone CGM transmits your glucose readings to a smartphone or reader device. It does not need to be connected to an insulin pump. If you don't have a compatible smartphone, Abbott and NZMS will supply standalone reader devices free of charge.
The standalone CGMs funded in Aotearoa New Zealand are:
- Dexcom One+
- FreeStyle Libre 2 (Note: This CGM is being discontinued but will still be funded until May 2026)
- FreeStyle Libre 2 Plus: (From 1 May 2025 this CGM will replace the FreeStyle Libre 2. People who are using the Freestyle Libre 2 will need to get a new prescription for the FreeStyle Libre 2 Plus. The size, phone app, reader, adhesive, and application are the same as the FreeStyle Libre 2.)
The CGMs work in the same way, but differ in size, look and some features. You may need advice on getting the most out of your CGM. As a guide, see
- Comparing stand-alone CGM Aotearoa(external link) Diabetes Collective
- Standalone CGMs comparison table(external link) Diabetes New Zealand.

Image credit: PHARMAC (with permission), NZ
An insulin pump is a small device that delivers insulin continuously under your skin. A pump can be used with a CGM to create an automatic insulin delivery (AID) system. This allows the pump to adjust the insulin dose automatically depending on readings from the CGM. Learn more about insulin pumps.
The insulin pump may also be used with an algorithm, which uses the signal from your CGM and figures out what your insulin needs are. It then adjusts the dose that your insulin pump delivers.
There are 2 funded insulin pumps in Aotearoa New Zealand. Both pumps are compatible with at least 2 types of continuous glucose monitor (CGM). If you qualify for a funded insulin pump, you can also get funded CGMs. You may need advice on getting the most out of your CGM. As a guide, see:
- Comparing pump compatible CGMs(external link) Aotearoa Diabetes Collective
- CGMs intraoperable comparison table(external link) on the Diabetes New Zealand website.
Your specialist diabetes team will be able to give you advice about insulin pumps and compatible CGMs.
Tandem T slim insulin pump works with:
- Dexcom G6
- Dexcom G7
The Tandem t:slim X2 will also work with the FreeStyle Libre 3 by July 2025.
The mylife Ypso insulin pump works with:
- Dexcom G6
- FreeStyle Libre 3 +
Note: The number of funded CGMs per patient varies by product. Find out more about how many CGMs do I get?(external link)
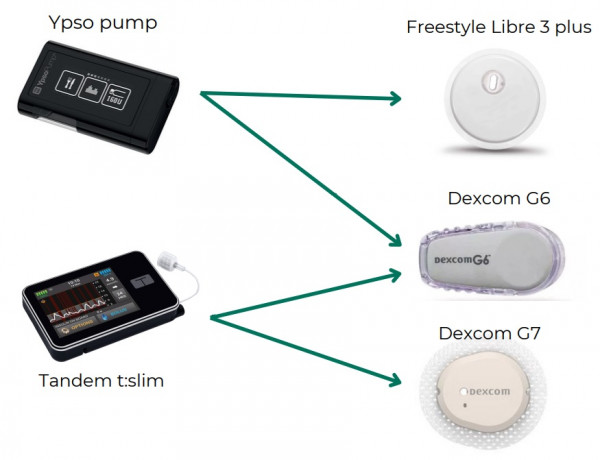
Image credit: PHARMAC (with permission), NZ
Note: The Tandem t:slim X2 will also work with the FreeStyle Libre 3 by July 2025.
More information- There are differences in how each CGM works. You may need advice on getting the most out of your CGM. As a guide, see device comparison tables(external link) of CGMs and insulin pumps by Diabetes New Zealand.
- For more information about the above CGMs see Dexcom CGMs(external link) and Freestyle Libres(external link).
- You can swap between the 2 funded CGMs when you get a new prescription. You don't need a new special authority. Just ask your prescriber to prescribe the other CGM.
You will usually have a training session with a diabetes nurse, a pharmacist, or with someone from the company who provides the device, to show you how to use it and how to make decisions on managing your diabetes based on the results.
Getting support
If you have any technical questions you can call:
- NZMS, for Dexcom CGM: 0508 634 103
- MediRay (Abbott) for FreeStyle CGM: 0800 106 100
Problems with the CGMs
- Faulty CGMs: If you're having trouble with your CGM or think it may be faulty, contact the supplier or your pharmacy for help. If it's faulty, the suppliers will provide you a replacement free of charge. Any CGMs provided to replace faulty ones would not count towards your annual limit.
Note: To replace a faulty sensor, the suppliers require you to supply the serial number from the box of the sensor (or you may be able to get this from the smartphone app if you have scanned the sensor at least once). Also, they may require you to return the faulty sensor. - Broken or lost CGMs: There's a limit on the total number of CGMs you can have each year that takes this into account. If you’ve used more than the limit, you may need to pay for more CGMs. Check with your healthcare provider how many CGMs you can get.
Travelling with diabetes
- Diabetes and travelling(external link) Diabetes New Zealand
- Navigating airport security screening – guidance for people living with diabetes(external link) Aviation Security Service, NZ
- Travelling with children who have diabetes(external link) KidsHealth NZ
- Travel(external link) Diabetes Australia
- Travel and type 1 diabetes(external link) Diabetes Australia
Finger prick readings are still very important to manage your diabetes. Using a CGM means you’ll need to do them much less often.
Finger prick readings measure the amount of glucose in your blood and gives a more accurate result of your current glucose level. CGM measures the amount of glucose in the fluid surrounding your cells which may be 2 to 10 minutes behind your blood glucose levels. It’s normal for these results to be a bit different.
Finger prick tests may be needed to help calibrate the CGM (check it's reading accurately) and at times when blood glucose levels are changing quickly (eg, if you're dehydrated, after doing extreme physical activity, or after certain foods or medicines).
You should still check your blood glucose level using a finger prick test when you are sick, and if:
- You have symptoms of low blood glucose but your CGM reads above 4 mmol/L: If the blood glucose level on your finger prick test is below 4 mmol/L, you're having a hypo and must treat it immediately. Read more about how to treat hypoglycaemia (low blood glucose).
- Your CGM reads below 4 mmol/L but you don't have symptoms of low blood glucose: Only treat yourself for a hypo if your blood glucose level on your finger prick test is below 4 mmol/L.
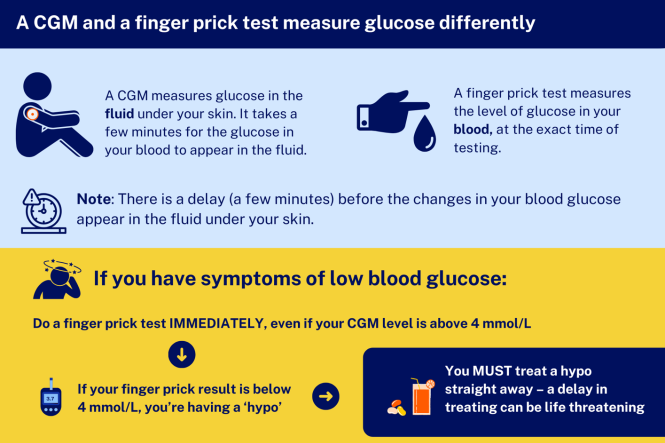
Image credit: Healthify He Puna Waiora
Read more about:
Your CGM has an adhesive tape that sticks to the skin, keeping the CGM in place. Some people using a CGM may get skin irritation at the site. This can include itch, redness, swelling and pain. It may be a problem if you have sensitive skin or skin problems such as eczema.
Possible causes
- An allergic reaction to the glue on the tape.
- The sensor being pressed too firmly against your skin.
- Skin irritation when removing the tape.
Tips when applying the sensor
- Ensure your skin is clean before you place your CGM. Use soap and water to clean your skin and remove any cream, oil or lotion. Then dry your skin well by patting with a towel.
- Wash your hands with soap and water before placing your CGM.
- If you use soap and water, it's not necessary to use alcohol or wipes as these can irritate your skin.
- Use a different site each time and allow a recently used site to rest for a few days before reusing it. Avoid areas with irritated or broken skin.
- If you have 2 devices taped to your skin, such as a CGM and an insulin pump, it may help to keep a diary to remind you about which sites you've used recently.
- Follow the device guide for applying the sensor and over-tape.
Tips when removing the sensor
- When removing the adhesive tape, you can use a water-based adhesive remover but cooking oil is also effective. Apply the oil 5 to 10 minutes before removing it.
- Gently and slowly remove the adhesive tape – avoid ripping it off quickly, as this can damage your skin.
If you have an ongoing skin reaction
If your skin is red and itchy after the CGM is removed, you can use a hydrocortisone cream or ointment that you can buy from your pharmacy. Don't use the cream or ointment for more than a few days (unless told to do so by a healthcare provider). If your skin reaction continues, talk to your healthcare provider – you may need to try a different type of CGM or use a skin barrier wipe. Also tell your healthcare provider if you have had eczema or any skin reactions to tapes.
Funding announced for continuous glucose monitors (CGMs) and insulin pumps(external link) Diabetes NZ
Continuous glucose monitors (CGMs) and insulin pumps(external link) Pharmac, NZ
Dexcom CGMs (external link)
FreeStyle Libre(external link)
Diabetes technology(external link) KidsHealth, NZ
Glucose monitoring in children with diabetes(external link) KidsHealth, NZ
Skin reactions with insulin pumps & CGM(external link) Aotearoa Diabetes Collective, NZ, 2025
Brochures
Navigating airport security screening(external link) Aviation Security Service New Zealand and Diabetes New Zealand
Which CGMs work with which insulin pump?(external link) PHARMAC, NZ, 2024
Skin reactions with insulin pumps & CGM(external link) Aotearoa Diabetes Collective, NZ
Apps
References
- Funding announced for continuous glucose monitors (CGMs) and insulin pumps(external link) Diabetes New Zealand, NZ, 2024
- Glucose monitoring in children with diabetes(external link) KidsHealth, NZ, 2022
- Continuous glucose monitoring(external link) Cleveland Clinic, US, 2021
- Monitoring your blood glucose(external link) Health New Zealand | Te Whatu Ora, NZ
- Blood sugar levels can fluctuate for many reasons(external link) Mayo Clinic, US, 2022
Brochures

Which CGMs work with which insulin pump?
PHARMAC, NZ, 2024

Skin reactions with insulin pumps & CGM
Aotearoa Diabetes Collective, NZ, 2025
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Claire Salter, Clinical Pharmacist, Tauranga; Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:






