Glue ear happens when your child's middle ear is filled with fluid. The fluid is thick and sticky, like glue. Glue ear can affect one or both ears. It often follows an ear infection or can happen on its own.
The image below has the parts of the ear labelled and show the location of the middle ear.
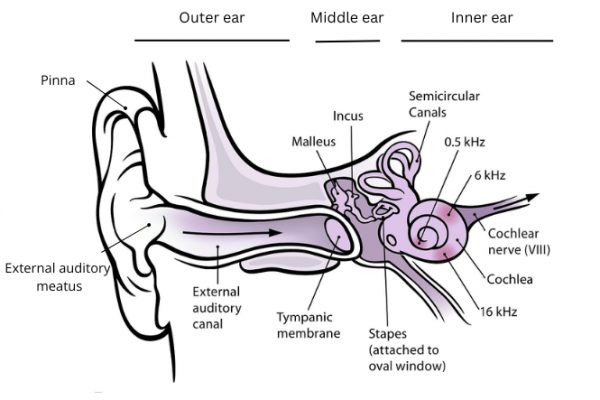
Image credit: Chittka L, Brockmann(external link) Wikimedia Commons with added labels
Read our page on ear infections to find out how fluid can build up in the middle ear. The risk factors for glue ear are the same as for ear infections.
After an ear infection, the fluid in the middle ear may stay around for weeks. This can happen even if your child has had antibiotics. The fluid clears up in 8 out of 10 children within 12 weeks. When there's still fluid for more than a couple of weeks, this is called glue ear.
The medical name for glue ear is OME (otitis media with effusion) or secretory otitis media. The video below shows how it develops and affects hearing.
Video: How glue ear develops
This video may take a few moments to load.
(BUPA, UK, 2013)






