Blood clots | poketoto
Key points about blood clots
- It’s normal for your blood to clot so it can stop the bleeding if one of your blood vessels is injured.
- However, blood clots (poketoto) can sometimes form inside blood vessels even when you're not bleeding and get stuck in places that can cause life-threatening problems.
- There are things you can do to reduce your chance of getting a blood clot, eg, taking anticoagulants.
- They can be treated if found early enough.
Video: Blood clots
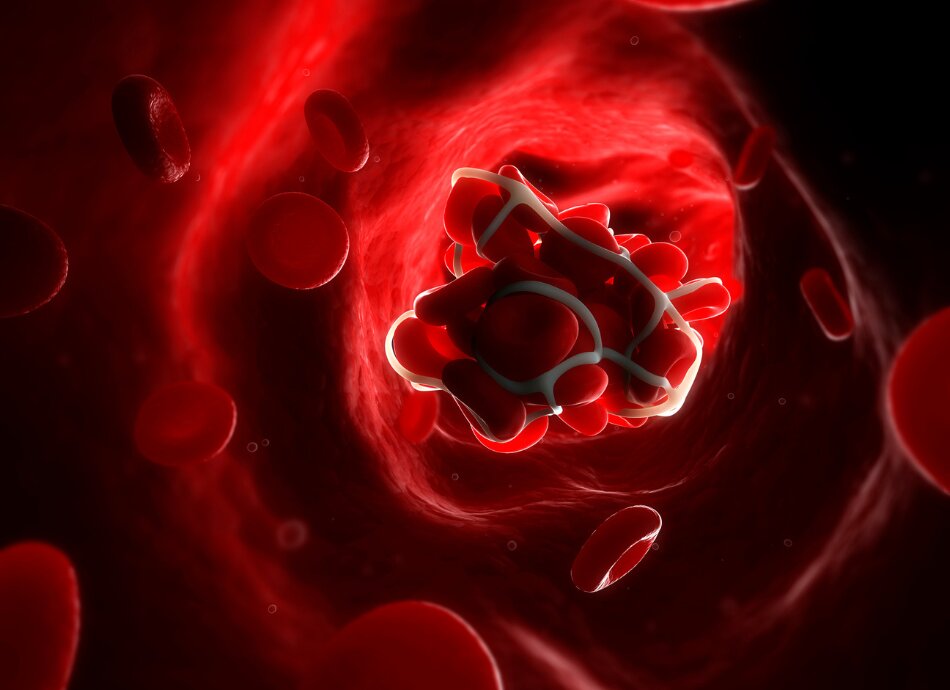
Blood clots form when your blood gets thicker and becomes semisolid. It’s a normal response when you are cut, the blood thickens and clots at the site of the injury and stops the bleeding. However blood can thicken and form a clot when there’s no injury and if it forms inside a blood vessel (called a thrombosis) and doesn’t dissolve (as it would after an injury has healed) it can break off and move around inside your blood vessels. If it gets stuck and blocks the flow of blood it can create problems.
A blood clot, or thrombus, can develop in your veins (which carry blood to your heart) or in your arteries (which carry blood away from your heart).
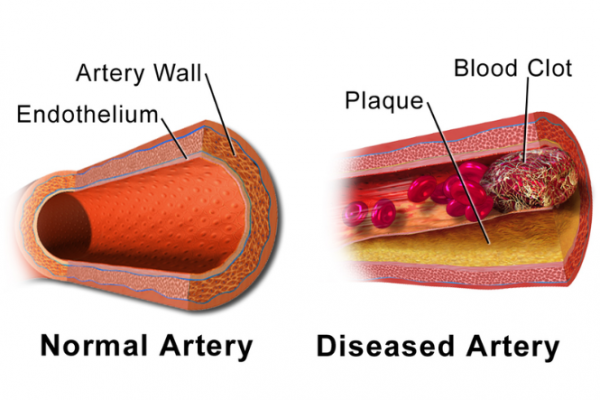
Image credit: Blausen Medical Gallery 2014 via Wikimedia Commons
- A blood clot in one of the veins deep in your legs is called a deep vein thrombosis (DVT).
- If a blood clot in a deep vein breaks off and travels through your bloodstream and through your heart to your lungs and blocks the blood flow there, it causes a pulmonary embolism.
- A blood clot can also form when the lining of your arteries has thickened making it harder for the blood to flow through. This can cause a heart attack, stroke, or transient ischaemic attack (TIA).
Some conditions, eg, genetic disorders and diabetes can make your blood clot too much or not dissolve properly.
If you’re taking oral contraceptives (the pill), smoking can also increase your risk of blood clots.
Most deep vein thrombosis (DVT) is caused by not being active enough, so it can often happen when you’re in hospital. Less often, it can happen if you fly on a long-haul flight or if you’re not able to walk around much because of illness, injury, or recent surgery – especially if you’ve had surgery on your hips or knees. Find out more about the causes of DVT.
Pulmonary embolism most often occurs when a blood clot in your leg travels to your lungs. Find out more about the causes of pulmonary embolism.
Arterial clots that lead to heart attacks, strokes and TIAs are caused by fatty deposits building up along the walls of your arteries over time, narrowing them, making it harder for blood to flow through them and causing inflammation in the walls of the blood vessels. When blood flow is sluggish or there is a lot of inflammation in a blood vessel, the blood tends to clot more easily. This is called cardiovascular disease.
The following factors increase your risk of developing a blood clot:
- Medical conditions affecting clotting, eg, a blood disorder, some heart conditions (eg, atrial fibrillation) or diabetes.
- Taking medicines that increase clotting risk, or that contain oestrogen, eg, hormone replacement or birth control pills, patches, or rings.
- Hospitalisation (or confinement to bed) for illness or surgery making you immobile for a long time.
- Major injury or surgery, particularly to the legs.
- Cancer and some cancer treatments.
- Pregnancy, and up to 6 weeks after the baby is born.
- The use of hormone replacement therapy (HRT) containing oestrogen.
- Varicose veins.
- A previous or family history of blood clots.
- Sitting too long, especially with legs crossed, eg, on a long-haul flight.
- Obesity.
- Smoking.
- Getting dehydrated.
- High blood pressure or high cholesterol.
Symptoms depend on where the blood clot has formed. Find out about symptoms of DVT, pulmonary embolism, heart attack, stroke and TIAs.
Diagnosis
Your symptoms will help your healthcare provider diagnose which type of blood clot you are being affected by. Find out about the diagnosis of DVT, pulmonary embolism, heart attack, stroke and TIAs.There are different treatments depending on what type of blood clot you have.
Treatment
There are different treatments depending on what type of blood clot you have.
You may be prescribed a medicine to dissolve the clot or stop it getting bigger. These medicines include anticoagulants, aspirin, clopidogrel. You may need surgery to remove the clot, or to widen your artery or bypass the blocked artery.
For more information on treatment, see our related topics pages on DVT, pulmonary embolism, heart attack, stroke or TIA.
What self-care can I do if I have blood clots?
If you have a DVT, wear your compression stockings as advised by your healthcare provider, and do advised DVT prevention exercises. Evidence suggests that mild to moderate exercise is safe if you have a DVT, especially if you’re on anticoagulants. Here’s a video to show you how to do some of them. It may take a few moments to load.
Video: DVT (deep vein thrombosis) prevention exercises
(Ask Dr Jo, US, 2016)
With any type of clot, take your medicines. If you’re on anticoagulants (medicines to reduce clotting) you’re more likely to bleed from small injuries so be careful when cutting your nails, and wear gloves when using sharp tools or gardening.
If you have a clot in your arteries, then follow the dietary advice of your healthcare provider. See coronary heart disease for more information.
Staying active with walking or swimming can assist the healing process but talk to your healthcare provider about what sort of exercise is right for you.
Don’t sit too long and ask whether it’s a good idea to keep wearing compression stockings for a while.
Watch your weight and stay well hydrated by drinking plenty of water.
What support is there for living with blood clots?
There are different organisations to support you, depending on the type of clot you have. See DVT, pulmonary embolism, heart attack, stroke or TIA.

Image credit: Healthify He Puna Waiora
You can reduce your risk of clots in your arteries (arterial thrombosis) if you:
- don't smoke cigarettes, especially if you are taking oral contraceptives
- exercise each day, keep moving
- eat heart healthy foods, eg, fruit and vegetables, lean meats and low fat dairy products
- lose weight if you are overweight or obese
- drink less, or no, alcohol
- stay well hydrated (drink plenty of water).
If you're at a high risk of getting a blood clot in your arteries, your healthcare provider may recommend medicine to reduce your cholesterol, blood pressure or the risk of your blood clotting.
If you're travelling, or in hospital, reduce the risk of DVT by wearing compression stockings, moving your feet and legs as much as possible (see the video in the self-care section), drinking plenty of water and taking blood thinners to prevent blood clots if advised by your healthcare providers.
For more information, see DVT, pulmonary embolism, heart attack, stroke or TIA.
Apps reviewed by Healthify
You may find it useful to look at some Exercise apps, Heart rate apps, and Stroke apps.
Thrombosis(external link) NHS Choices, UK,
Arterial thrombosis(external link) NHS Choices, UK
Apps
Exercise apps
Heart rate apps
Stroke apps
Brochures
Preventing blood clots – information for patients and carers(external link) Clinical Excellence Commission, Australia
References
- An update on antithrombotic medicines – what does primary care need to know?(external link) Best Practice Journal, NZ, 2015
- Inherited causes of blood clots(external link) Indiana Hemophilia and Thrombosis Center, US, 2017
- Smoking prevention and cessation in adolescents – changing futures, saving lives(external link) Best Practice Journal, NZ, 2013
- Blood clots – symptoms and causes(external link) Heart Research Institute, NZ
- Dos and don’ts after a blood clot(external link) WebMD, US, 2022
- Diagnosing and managing venous thromboembolism – what can you do to improve patient care in your clinical practice?(external link) National Blood Clot Alliance, US
- Fact vs fiction – exercising after a blood clot(external link) North American Thrombosis Forum, US
Management of blood clots
Suspected DVT
The Royal Australian and New Zealand College of Radiologists recommends that you don’t request duplex compression ultrasound for suspected lower limb deep venous thrombosis in ambulatory outpatients unless the Wells Score (deep venous thrombosis risk assessment score) is greater than 2, OR if less than 2, D-dimer assay is positive. For more details, see the Choosing Wisely recommendations(external link).
Suspected pulmonary embolism
The Royal Australian and New Zealand College of Radiologists recommends that you don’t request any diagnostic testing for suspected pulmonary embolism (PE) unless indicated by Wells Score (or Charlotte Rule) followed by PE Rule-out Criteria (in patients not pregnant). Low-risk patients in whom diagnostic testing is indicated should have PE excluded by a negative D-dimer, not imaging. For more details, see the Choosing Wisely recommendations(external link).
Also see our related healthcare provider pages on each condition: DVT, pulmonary embolism, heart attack, stroke or TIA.
Resources
The role of thrombophilia testing in general practice(external link) BPAC, NZ, 2011
Tran HA, Gibbs H, Merriman E, et al. New guidelines from the Thrombosis and Haemostasis Society of Australia and New Zealand for the diagnosis ad management of venous thromboembolism(external link) MJA 2019;210(5)
Apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator.
Last reviewed:





