Morphine
This information is intended for use ONLY after you have been prescribed morphine.
Key points about morphine
- Morphine is used for the relief of moderate to severe pain such as that caused by an injury or operation, or by a terminal illness such as cancer.
- It may also be used to ease breathlessness or cough in palliative care.
- Follow the instructions on the label of your medicine, for how much to take and how often.
- Find out how to take it safely and possible side effects.

Morphine is used for the relief of moderate to severe pain such as:
- after an injury or operation
- pain caused by a terminal illness such as cancer.
It's usually used when milder pain medicines such as paracetamol or non-steroidal anti-inflammatories (NSAIDs), don’t work well enough.
- Morphine belongs to a group of medicines called opioids. They act on your brain and nervous system to reduce pain.
- Other types of pain relievers such as paracetamol and NSAIDs (ibuprofen, diclofenac, naproxen) may also be used with morphine.
- Read more about pain, pain-relief medication, and opioids.
Morphine is also used to treat breathlessness and cough in palliative care. A regular small dose may help to ease symptoms of shortness of breath. Learn more about breathlessness in palliative care and cough in palliative care.
Morphine is also called:
- Sevredol tablets
- m-Eslon SR capsules
- RA-Morph liquid
- Wockhardt morphine liquid
- Oramorph.
Some types of morphine are short-acting or immediate release (eg, Sevredol tablets and morphine liquid) – they work quickly to ease your symptoms. Long-acting or slow release morphine (eg, m-Eslon SR capsules) works slowly over several hours to give a constant and more even pain control.
The dose of morphine will be different for different people.
- Some types of morphine are short-acting or immediate release (eg, Sevredol tablets and morphine liquid) – they work quickly to ease your symptoms.
- Long-acting or slow release morphine (eg, m-Eslon SR capsules) works slowly over several hours to give a constant and more even pain control.
- Always take your morphine exactly as your doctor has told you. Depending on the cause of your pain, your doctor may advise you to take regular doses or to take morphine only when you need it for pain relief. Make sure you know which is right for you.
- The doses of morphine used for breathlessness and cough are much lower than would be used for pain.
- The pharmacy label on your medicine will tell you how much to take, how often to take it, and any special instructions.
- If you’re drowsy or sleepy, don’t take your next dose until you’re wide awake. Ask your healthcare provider for advice.
Morphine is available as tablets, capsules, oral liquid and injections. Injections are mostly used in hospital.
- Follow the instructions on the label of your medicine, for how much to take and how often.
- You can take morphine with or without food.
- Some types of morphine are short-acting or immediate release and others are long-acting or slow release. Ask your pharmacist if you're not sure about the type you're taking.
- If you're taking it regularly and forget to take your dose, take it as soon as you remember that day. But if it's nearly time for your next dose, just take the next dose at the right time. Do not take double the amount.
| Formulation | How to take it |
| Tablets – an example is Sevredol® tablets |
|
| Capsules –
an example is m-Eslon SR |
|
| Oral liquid –
Examples are RA-Morph and Wockhardt morphine |
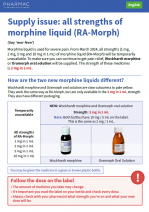
Morphine liquid is available in many strengths.
|
Here are some things to know when you're taking morphine. Other things may be important as well, so ask your healthcare provider what you should know about.
Eat plenty of fibre and drink more water while you are taking morphine
- Morphine can affect your bowel movements – it might be hard or painful to poo (constipation).
- If this happens, ask your healthcare provider for a laxative, to soften your poo.
- Eating foods with fibre, drinking plenty of water and keeping active can help.
Morphine can make you sleepy, drowsy, dizzy or affect your concentration
- If you’re drowsy or sleepy, don’t take your next dose until you’re wide awake. Ask your healthcare provider for advice.
- Limit or avoid alcohol as it can make these effects worse.
- Don’t drive a vehicle, ride a bike or operate machinery (including power tools) and don’t make important personal or business decisions or sign legal papers.
Taking other medicines
- Your doctor may recommend taking other pain relievers such as paracetamol and NSAIDs (ibuprofen, diclofenac, naproxen) as well. If taken regularly, they can reduce the amount of morphine you need to take.
- If you're taking any other medicines, or starting a new medicine, check with your doctor or pharmacist to make sure they're safe to take with morphine. This includes any medicines you buy without a prescription (over the counter), such as herbal and complementary medicines or recreational drugs.
- If your pain isn’t improving don’t take extra doses. If you’re also prescribed paracetamol or anti-inflammatories, you can use them with morphine. If you're not sure, ask your healthcare provider.
- Try other ways to manage your pain. Morphine reduces severe pain but won’t take all of your pain away. Try relaxation techniques, gentle exercises and stretches.
If you’re breastfeeding
- Most people can continue to breastfeed while taking morphine for pain relief.
- Let your healthcare providers know you’re breastfeeding so they can discuss this with you.
- It’s recommended you avoid co-sleeping with your baby when taking morphine. Put your baby to sleep in their own bed.
Morphine is addictive
- If you're addicted to morphine, you may find it difficult to stop taking it or feel you need to take it more often than necessary.
- It's unusual for people who are prescribed morphine for a short time or for a terminal illness to become addicted to it.
- Some people are more likely to develop addiction than others and seem to be very sensitive to the cravings. You may be at risk for addiction if you have mental health problems (such as depression) or a history of substance abuse, including alcohol and recreational drugs.
- To reduce your risk of addiction when using morphine for short-term pain relief, use it for the shortest possible time, at the lowest effective dose.
- Have a plan in place for how and when to reduce and stop taking morphine.
- Talk to your doctor if you're worried about addiction or if you want to know more about how to prevent withdrawal symptoms.
Like all medicines, morphine can cause side effects, although not everyone gets them. Often side effects improve as your body gets used to the new medicine.
| Side effects | What should I do? |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
Medsafe Consumer Information Sheet: Arrow-Morphine LA(external link)
New Zealand Formulary Patient Information: morphine (short acting)(external link) morphine (long acting)(external link)
Brochures
Understanding morphine and other opioid medicines [PDF, 2.6 MB] Palliative Outcome Initiative English [PDF, 2.6 MB], Korean [PDF, 1.8 MB], Samoan [PDF, 1.4 MB], Simplified Chinese [PDF, 1.3 MB], Tongan [PDF, 1.2 MB]
Risks of opioid medicines(external link) Medsafe,NZ
Managing pain and opioid medicines(external link) NPS MedicineWise & Choosing Wisely Australia
Morphine [PDF, 208 KB] Mary Potter Hospice, NZ, 2018 English [PDF, 208 KB], Cook Island [PDF, 206 KB], Samoan [PDF, 206 KB], Tongan [PDF, 207 KB], Tokelauan [PDF, 206 KB]
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ English(external link), te reo Māori(external link)
Opioid medicines for short-term pain [PDF, 105 KB] Healthify He Puna Waiora, NZ English [PDF, 105 KB], te reo Māori [PDF, 126 KB]
Morphine supply issue – RA-Morph liquid to be replaced by Wockhardt morphine liquid [PDF, 183 KB] PHARMAC, NZ English(external link), te reo Māori(external link), Tongan(external link), Samoan(external link), Cook Islands Māori(external link)
References
- Morphine salts(external link) New Zealand Formulary
Brochures
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated: