If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Medicines for nausea and vomiting
Also called anti-sickness medicines or antiemetics
Key points about nausea and vomiting medicines
- There are a number of different medicines that can help when you feel sick (nausea) or are being sick (vomiting).
- Your healthcare provider will recommend a medicine for your nausea or vomiting depending on what’s causing your symptoms.
- Find out which nausea and vomiting medicines are used for different conditions.

Nausea (feeling sick) and vomiting (being sick) can be caused by many things such as pregnancy, motion sickness, Ménière's disease, migraines and some medicines such as chemotherapy.
Taking a medicine to treat nausea and vomiting may not always be the best option, so talk to your healthcare provider first. Read more about nausea and vomiting.
There are a number of different medicines that can help treat nausea and vomiting. These medicines are called anti-sickness medicines or antiemetics. The choice of treatment depends on factors such as:
- what has caused your nausea and vomiting
- whether you have any other medical conditions or are taking any other medicines
- whether you're pregnant
- your age
- possible side-effects of the medicines.
Many different conditions can cause nausea, and there are a range of treatments that could be prescribed. The sections below are a guide.
Medicines for motion sickness are usually taken before you start travelling, to prevent you from becoming sick, rather than taking the medicine after the nausea or vomiting develops.
In Aotearoa New Zealand, you can buy medicines for motion sickness over the counter in a pharmacy after a consultation with a pharmacist.
A commonly used medicine to prevent motion sickness is hyoscine (also called scopolamine), which is a patch that you apply to the skin, behind the ear, at least 5 hours before the journey. Each patch lasts up to 72 hours (3 days). It can cause drowsiness, so avoid using it if you're driving. Read more about hyoscine.
Cyclizine, meclozine and promethazine are available as tablets and should be taken at least 1 to 2 hours before departing. They can make some people feel drowsy, sleepy or tired. Don't drive until you know how the medicine affects you. Read more about cyclizine, meclozine and promethazine.
Betahistine is used to relieve the symptoms associated with Ménière's disease such as dizziness, vertigo, loss of balance and ringing in your ears (tinnitus). It's unlikely to stop all these symptoms, but it may reduce how often they occur and their severity.
Your healthcare provider may advise you to try betahistine for 6 to 12 months to see if it helps to reduce your symptoms. If it does, it can be continued. Read more about betahistine.
Other medicines such as cyclizine and prochlorperazine can be used for short-term relief of symptoms. Prochlorperazine is usually used for severe symptoms when other medicines haven't been effective.
Most people with migraine headaches get nausea or vomiting. Medicines used to ease these symptoms are metoclopramide, domperidone and prochlorperazine. They can be helpful to treat migraine even if you don't experience nausea or vomiting and can be used together with other pain relievers and triptans.
As with pain relievers, anti-sickness medicines work better if taken as soon as your migraine symptoms begin. Read more about migraine and medicines for migraine.
During early pregnancy nausea and vomiting are common. This is often called "morning sickness" even though symptoms can occur at any time of the day and may continue for the whole pregnancy. These symptoms are generally mild and don't need medicine.
Severe vomiting in pregnancy is known as hyperemesis gravidarum. It's much worse than regular morning sickness. There are a number of anti-sickness medicines that you may be offered such as cyclizine, promethazine, prochlorperazine, metoclopramide and ondansetron. These medicines are not all licensed for use in pregnancy, but there's no evidence that they're harmful to your baby.
Always check with your healthcare provider before taking any medicine or supplement when you're pregnant.
Some types of chemotherapy can cause nausea and vomiting. Depending on the type of chemotherapy, these feelings can occur while you're receiving the medicine, right after, or many hours or days later.
Not everyone feels sick after chemotherapy. How likely you are to develop nausea and vomiting depends on many things such as:
- the types of chemotherapy medicine given
- the dose (high doses of chemo are more likely to cause nausea and vomiting)
- how often the medicine is given – for example, if doses of a chemo medicine that causes nausea and vomiting are given close together, there’s less time for the person to recover from the effects of the last dose before the next one is given
- how the medicines are given – for example, chemotherapy given into a vein (intravenous, or by IV) may cause nausea and vomiting much faster than a medicine given by mouth. This is because the medicine given by IV is absorbed faster
- individual differences – not every person will have the same response to a dose or type of chemotherapy.
It’s easier to prevent nausea and vomiting than it is to try and stop it once it's developed.
Medicines used to prevent and treat chemotherapy-related nausea in Aotearoa New Zealand include ondansetron, often combined with dexamethasone, and sometimes aprepitant for more severe cases.
There is no anti-sickness medicine that can prevent or control chemo-related nausea and vomiting 100% of the time. This is because chemotherapy acts on the body in different ways, and each person responds to medicines differently.
Your healthcare provider will discuss the best options for you and work on a treatment plan to control your symptoms.
Brochures
Medicines and side effects(external link) Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications (external link)Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- Drugs used in nausea and vertigo(external link) New Zealand Formulary
- Hyoscine hydrobromide(external link) New Zealand Formulary
- Antiemetics(external link) New Zealand Formulary
Brochures
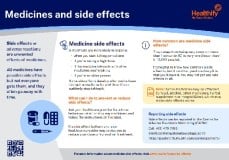
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Stephanie Yee, Pharmacist, Auckland
Last reviewed:





