Wishing everyone a safe and happy Christmas and New Year – Meri Kirihimete from the Healthify team.
Intrauterine devices (IUD) for heavy periods
Key points about intrauterine devices (IUDs) for heavy periods
- An intrauterine device (IUD) can be used for the treatment of endometriosis and heavy periods (also called menorrhagia).
- The intrauterine device (IUD) for these conditions contains a hormone and is commonly called Mirena®.
- Find out how Mirena is used to treat these conditions and possible side effects.

In Aotearoa New Zealand Mirena® is the intrauterine device (IUD) used for the treatment of heavy periods or excessive menstrual bleeding (also called menorrhagia).
IUDs are often used for contraception to prevent pregnancy, but Mirena is also used as a treatment for heavy or painful periods, even for women who don't need contraception.
Mirena is also sometimes used for endometriosis. It’s not approved for this by Medsafe (New Zealand's agency for licensing medicines) so if your healthcare provider recommends it, they'll talk to you about the risks and benefits of this medicine so you have enough information to make a decision about using it ‘off-label’. Read more about unapproved medicines.
Note: The information on this page is about Mirena for heavy periods and endometriosis. For information about Mirena for contraception, see IUDs for contraception.
Mirena is a small, white T-shaped plastic device with a stem attached to 2 removal threads that is placed inside your womb (uterus). It slowly releases the hormone progestogen (as levonorgestrel). This makes the lining of your womb thinner, making you less likely to have menstrual bleeding and reducing heavy, painful periods.
Once it's put in, Mirena lasts for up to 5 years. It can be put in at your GP clinic and you generally don’t need an operation or a general anaesthetic for this.
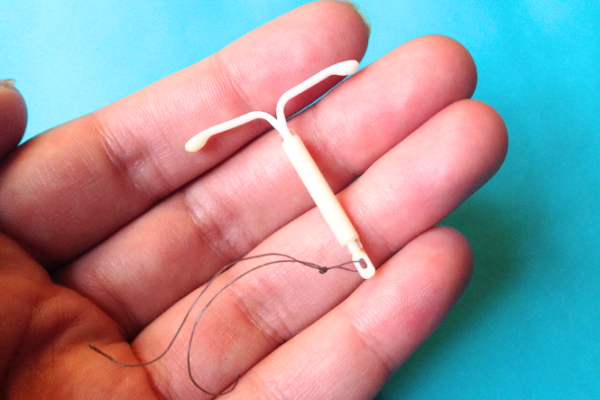
Image credit: Sarahmirk via Wikimedia Commons(external link)
The number of spotting and bleeding days may increase when you first have a Mirena put in. This can last for a few days or weeks but then the amount of bleeding you have during your periods slowly decreases.
It can take a few months for Mirena to reach its full effect, but by 6 months, most people only have light bleeding and sometimes no bleeding at all. Bleeding may also be irregular.
The IUD can be put in at any time but you should only have an IUD put in if it’s certain you’re not pregnant or don’t have a sexually transmitted infection such as chlamydia or gonorrhoea.
The IUD is usually put in towards the end of a period or shortly afterwards, to ensure you’re not hapū. You can also be advised to get one 4 to 6 weeks after your pēpi is born, or straight after an abortion.
Before the IUD is put in, you'll need to have a vaginal examination. The doctor or nurse will check the size and position of your womb (uterus).
The IUD is then put in using a small plastic device.
- Putting in an IUD can sometimes be uncomfortable. Read more about discomfort or pain during the fitting of an IUD.
- Light vaginal bleeding may also occur for a short while afterwards. Use pads rather than tampons or menstrual cups for the first few days after your IUD is put in.
- It’s also recommended to avoid sex, swimming and baths for the first few days after a Mirena is put in.
- Your healthcare provider will usually want to check that there are no problems a few weeks after an IUD is put in. This is best done after your next period. After this, there is no need for any routine check until it is time to remove the IUD. However, contact your healthcare provider at any time if you have any problems or queries.
- Most people have no problems, and the IUD can remain in place for up to 5 years.
Read more about intrauterine devices (IUDs)(external link) including how to prepare for your appointment and what to expect after your IUD appointment.
Checking the IUD is in place
- The IUD can come out of your uterus (also called expulsion): A small number of people find that the IUD can come out of their uterus. The risk is higher if you:
- are a teenager
- have heavy menstrual bleeding
- have a high body mass index (BMI)
- have an IUD put in immediately after childbirth.
- If the IUD comes out, it's no longer effective. You may be able to have a new IUD fitted.
- You’ll be taught how to feel for the threads of the IUD so you can check it’s in place. It’s best to check the threads regularly, after each period or at the beginning of each calendar month.
- If you can’t feel the thread, it doesn't necessarily mean that the IUD has fallen out. Sometimes the thread is just difficult to feel or has been pulled up into the cervical canal (which won’t harm you).
- Contact your healthcare provider if you can’t feel the IUD thread.
Other information
- Other medicines: The levonorgestrel in Mirena interacts with some medicines (eg, anti-seizure medicines such as carbamazepine, lamotrigine or HIV medicines), herbal supplements (eg, St John’s Wort) and rongoā Māori, so check with your healthcare provider before starting any new medicines or supplements.
- Replacement: Mirena works for a maximum of 5 years. At the end of this time, you'll need to visit your healthcare provider to see if it needs to be replaced with a new one.
- Pregnant: If you become pregnant, contact your healthcare provider.
- Sexually transmitted diseases: the IUD does not protect you from sexually transmitted infections (STIs).
- Removal: The IUD can be taken out at any time if you’d like it removed. This needs to be done by a trained healthcare provider.
Any pain or discomfort you feel during and after an IUD is put in or removed is different for everyone.
If you’re worried about pain or discomfort it’s a good idea to talk to your healthcare provider beforehand to discuss your options.
You can take a support person with you during the insertion and removal of the IUD.
When the IUD is put in
Most people feel discomfort or pain. The type of IUD (hormonal or copper), your pain tolerance, and whether you’ve given birth before can influence how painful it feels.
The pain might feel like cramping or a sharp pinch that lasts for a few minutes. Some compare it to a strong period cramp.
To help reduce pain during the procedure, your healthcare provider may suggest taking over-the-counter pain relievers such as paracetamol and ibuprofen about 1 hour before the procedure.
It’s important to tell your healthcare provider if you’re having pain during the procedure.
Video: IUD insertion and pain – what to expect with Dr McNamee
(Sexual Health Victoria, Australia, 2023)
After the IUD is put in
It's common to experience cramping after the IUD has been put in. For some people the cramps may be mild and go away within a few hours. Others may have stronger period-like cramps for a few days afterwards.
The cramps can vary, but they usually lessen over time. You can use pain relievers such as paracetamol and ibuprofen. A hot water bottle or heat pad may also help.
If you have a sudden and severe attack of pain or any continuous lower abdominal pain, you should seek medical advice.
During removal of the IUD
The pain level when removing an IUD can also vary from person to person. Some people get mild discomfort or cramping, while others might feel stronger pain.
The removal process usually only takes a few minutes, and while it may feel uncomfortable, it's generally quick.
Some people may be advised to take pain relief before the removal of the IUD to help with pain and discomfort. If the IUD is difficult to remove or embedded, it might require additional steps, which can be more uncomfortable.
Like all medicines Mirena can cause side effects, although not everyone gets them.
| Side effects | What should I do? |
|---|---|
|
|
|
|
|
|
|
|
|
|
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
The following links have more information about Mirena®.
Mirena(external link) Medsafe Consumer Information, NZ
Brochures
Mirena – your questions answered(external link) Bayer New Zealand Limited, 2022
Medicines and side effects [PDF, 91 KB] Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- (external link)Levonorgestrel (implant)(external link) New Zealand Formulary
- Mirena(external link) Medsafe datasheet, NZ
- News item – access to levonorgestrel intrauterine devices/systems widened(external link) BPAC, NZ, 2019
- Long-acting contraceptives – implants and IUDs(external link) BPAC, NZ, 2021
- Intrauterine devices and uterine perforation(external link) Medsafe, NZ, 2014
- Instructions for hormonal IUD for heavy bleeding(external link) Sexual Wellbeing Aotearoa, NZ, 2024
- Pain associated with insertion of intrauterine contraception(external link) Faculty of Sexual and Reproductive Healthcare, Royal College of Obstetricians and Gynaecologists, UK, 2021
- Advice after you have a coil fitted(external link) NHS, UK, 2021
Brochures

Bayer New Zealand Limited, 2022

Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

5 questions to ask about your medications
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland.
Last reviewed:





