You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Intrauterine devices (IUDs) – commonly asked questions
Key points about intrauterine devices (IUDs) – common questions
- Here are some answers to common questions about intrauterine devices (IUDs).
- Learn more about the different types of IUDs and what to expect when they're put in.
- Find out how they work and possible risks and side effects.

The intrauterine device, or IUD, is a small, T-shaped plastic device made of a stem attached to threads which hang down through your cervix into your vagina. The IUD is placed inside your uterus (womb).
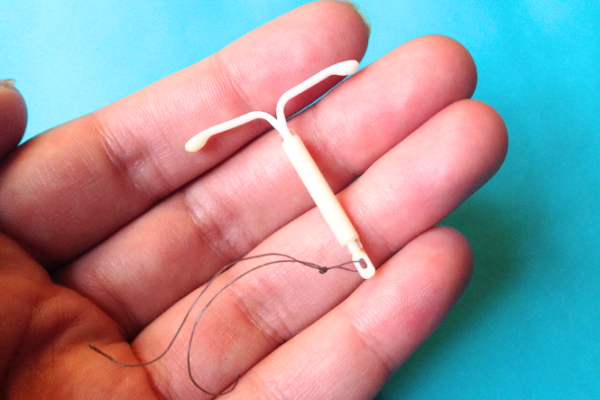
Image credit: Saramirk via Wikimedia Commons(external link)
There are 2 main types of IUDs available in Aotearoa New Zealand:
- Hormonal IUDs – these contain a progestogen hormone called levonorgestrel. Examples are Mirena® and Jaydess®.
- Copper IUDs – these are also called non-hormone IUDs.
Mirena and Jaydess are hormonal IUDs. They contain the hormone progestogen (as levonorgestrel).
Mirena
- Mirena contains 52 mg levonorgestrel. It's used for contraception to prevent pregnancy.
- It's effective for 5 years.
- At the end of this time, your IUD needs to be changed. Read more about IUDs for contraception.
- Mirena is also used for the treatment of heavy periods (menorrhagia) or excessive menstrual bleeding.
- Over time, the use of Mirena greatly reduces menstrual flow (bleeding) for many women. Read more about IUDs for heavy periods.
Jaydess
- Jaydess contains 13.5 mg levonorgestrel. It's used for contraception to prevent pregnancy and is effective for 3 years.
- At the end of this time, your IUD needs to be changed. Read more about IUDs for contraception.
The copper IUD is used for contraception to prevent pregnancy.
Long-term contraception: Copper IUDs last for 5 to 10 years, depending on the type used. Copper IUDs are used when hormonal contraceptives aren't recommended, such as for people who have had previous breast cancer or have some heart conditions.
Emergency contraception: Copper IUDs are also used for emergency contraception. A copper IUD can be put in up to 5 days after unprotected sex, or within 5 days of your earliest expected date of ovulation. The copper IUD may then either be removed after your next period or used as long-term contraception. Read more about emergency contraception.
The IUD is put into your womb (uterus) by an experienced healthcare provider.
This takes about 5 to 10 minutes, but your appointment will take about 30 minutes. During this time the healthcare provider will explain how the insertion is done and will give you instructions about what to expect once your IUD is in place.
Read more about how an IUD is put in.
After it's put in, you can’t feel the IUD or tell it's there, except by checking for the threads. The threads come out of your cervix and curl up inside the top of your vagina – they don’t hang outside your vagina.
If you're having penis-in-vagina sex, your partner shouldn’t be able to feel the IUD or the threads.
When you would like to stop using the IUD, or if it's due to be replaced, your healthcare provider will remove it during a pelvic exam. They will find the strings with an instrument and gently pull out the IUD.
Removal of an IUD usually takes less time than IUD insertion.
Any pain or discomfort you feel during and after an IUD is put in or removed is different for everyone. If you’re worried about pain or discomfort, talk to your healthcare provider beforehand to discuss your options.
You can take a support person with you during the insertion and removal of the IUD.
When the IUD is put in
Most people feel some discomfort or pain. The type of IUD (hormonal or copper), your pain tolerance, and whether you’ve given birth before can influence how painful it feels.
The pain might feel like cramping or a sharp pinch that lasts for a few minutes. Some people compare it to a strong period cramp.
To help reduce pain your healthcare provider may suggest taking over-the-counter pain relievers such as paracetamol and ibuprofen about one hour before the procedure.
It’s important to tell your healthcare provider if you’re having pain during the procedure.
Video: IUD insertion and pain – what to expect with Dr McNamee
(Sexual Health Victoria, Australia, 2023)
After the IUD is put in
It's common to experience cramping after the IUD has been put in. You may have mild cramps that go away within a few hours, or you may have stronger period-like cramps for a few days afterwards.
The intensity of the cramps can vary, and they usually lessen over time. You can use pain relievers such as paracetamol and ibuprofen. A hot water bottle or heat pad may also help.
If you have a sudden and severe attack of pain or any continuous lower abdominal pain, you should seek medical advice.
During removal of the IUD
The pain when removing an IUD can also vary from person to person. Some people get mild discomfort or cramping, while others might feel stronger pain.
The removal usually only takes a few minutes, and while it may feel uncomfortable, it's generally quick.
You may be advised to take pain relief before the removal of the IUD to help with discomfort or pain. If the IUD is difficult to remove or embedded, it might require additional steps, which can be uncomfortable.
Most people notice some changes to their period. This is normal and not harmful.
With a copper IUD, your periods might be longer, heavier and more painful, especially in the first few months. This usually gets better with time. Read more about possible side effects of IUDs for contraception.
With a hormonal IUD (Mirena or Jaydess), you might have spotting in the first few months and then light or no periods. Some people experience other side effects, including headaches and mood changes. Read more about possible side effects of hormonal IUDs.
Serious complications from IUDs are rare. However, some people do have problems. These problems usually happen during or soon after insertion.
- The IUD comes out of your uterus (also called expulsion): In a small number of people, the IUD may come out of your uterus. The risk is higher in teenagers, women with heavy menstrual bleeding, women with a high body mass index (BMI) and women who have an IUD put in immediately after childbirth. If the IUD comes out, it's no longer effective. You may be able to have a new IUD put in.
- Perforation: The IUD can go through the wall of your womb during placement. This is rare and occurs in only about 2 out of every 1,000 insertions. It usually doesn't cause any major health problems, but the IUD needs to be removed.
Yes, you'll be able to get pregnant as soon as the IUD is taken out.
Pregnancy is very rare with an IUD in place. If you do get pregnant with an IUD in, there's no extra risk for your baby, but there is a risk of complication in the pregnancy if it stays in. If you think you might be pregnant, talk to your healthcare provider as soon as possible. It's best to remove the IUD within the first 12 weeks of pregnancy.
The following links provide further information about IUDs:
Long-acting reversible contraception(external link) Sexual Wellbeing Aotearoa, NZ
Intra-uterine Device (IUD)(external link) Sexual Wellbeing Aotearoa, NZ
Mirena(external link) Medsafe Consumer Information, NZ
Jaydess(external link) Medsafe Consumer Information, NZ
Contraception – the copper IUD Family Planning NSW, Australia Arabic(external link), Chinese(external link), Farsi(external link), Korean(external link), Thai(external link), Vietnamese(external link)
Brochures
The IUD – intra uterine device(external link) Sexual Wellbeing Aotearoa, NZ
Jaydess – frequently asked questions(external link) Bayer New Zealand Limited
Mirena – your questions answered(external link) Bayer New Zealand Limited
References
- Intra-uterine contraception(external link) New Zealand Formulary
- Copper intra-uterine device(external link) New Zealand Formulary
- Levonorgestrel (intra-uterine system)(external link) New Zealand Formulary
- Long-acting contraceptives – implants and IUDs(external link) BPAC, NZ, 2021
- 2023 Update on long-acting reversible contraceptives(external link) Research Review, NZ, 2023
- Intrauterine devices and uterine perforation(external link) Medsafe, NZ, 2014
- Pain associated with insertion of intrauterine contraception(external link) The Faculty of Sexual and Reproductive Healthcare of the Royal College of Obstetricians and Gynaecologists, UK, 2021
- After you have a coil fitted(external link) NHS, UK, 2021
Brochures
Sexual Wellbeing Aotearoa, NZ, 2024
Bayer New Zealand Limited, 2023

Bayer New Zealand Limited, 2022
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland.
Last reviewed:





