Medicines for rheumatoid arthritis (RA) are used to relieve pain, reduce swelling and slow or stop joint damage.
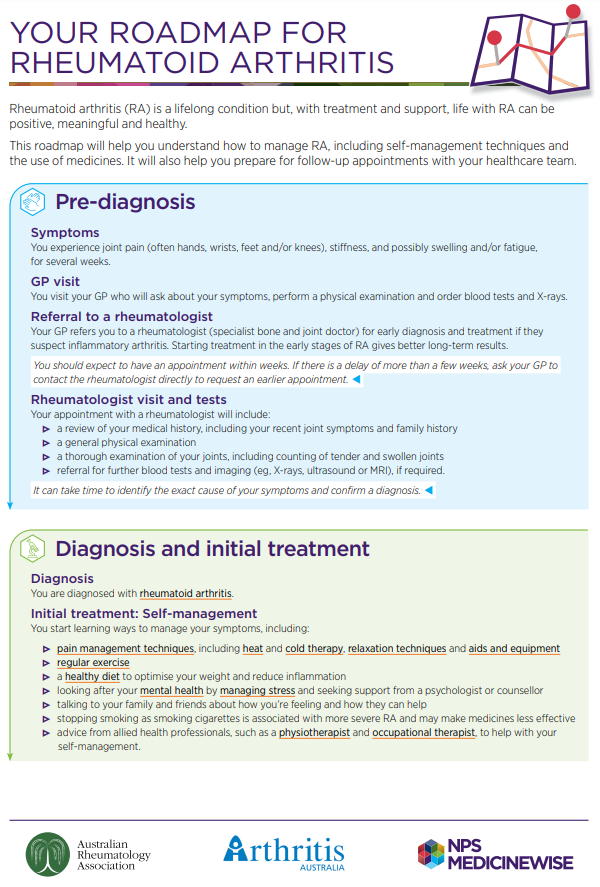
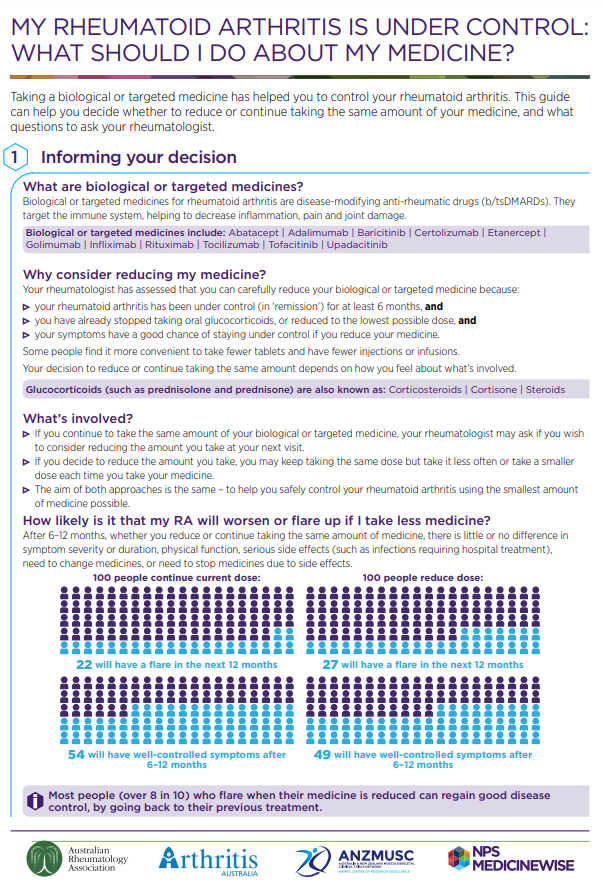
Each person responds differently to arthritis medicines. This means you need to work with your rheumatologist (a doctor who specialises in arthritis and related conditions) to identify the treatment that works best for you. You may need to try different treatments before finding the one that is right for you.
Common medicines for rheumatoid arthritis include:
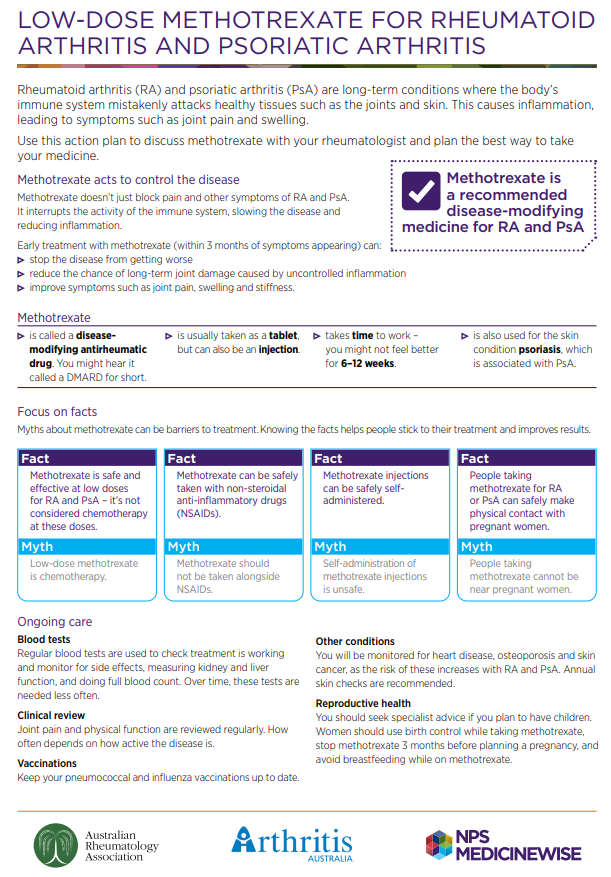
- Disease-modifying anti-rheumatic drugs (DMARDs)
- Pain relief medicines (paracetamol and codeine)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids (also called steroids)