Driving and medicines
Key points about driving and medicines
- Some prescription and over-the-counter (OTC) medicines can affect you in a way that makes it unsafe for you to drive.
- Be careful when driving until you know how your medicine affects you.
- Don't drive if your medicine impairs your ability to drive. Check how you feel before getting into your vehicle.
- In Aotearoa New Zealand it's against the law to drive while impaired.
- Read about how medicines can affect driving.

| How to make sure you are safe to drive |
|
If you're taking medicines and thinking of driving:
✔ Ask your doctor or pharmacist if the medicine you are given affects driving and whether it is safe for you to drive. |
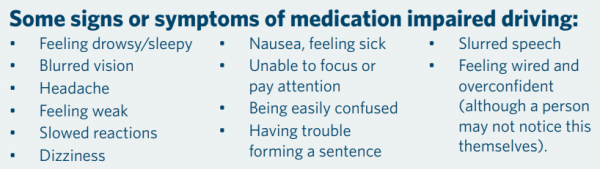
Some medicines can affect your concentration (how you focus or pay attention). They can slow your reaction times and cause sleepiness, blurred vision, dizziness, slowed down movements and fainting, or make you feel anxious or jittery. Do not drive if you have any of these.
If you think your medicines are affecting your driving, don't stop taking them or alter the dose without talking to your doctor or pharmacist first.
Don't drive if you have missed a dose of medicine that you need to control symptoms that could affect your driving.
- Epilepsy – some people with epilepsy may not be able to drive at all without taking regular medicines. Read more about driving with epilepsy.
- Diabetes – drivers with diabetes need to take regular medicines as prescribed because your blood glucose levels may get too high if you miss doses. You shouldn't drive if your blood glucose is too high (hyperglycaemia). High blood glucose levels can make you feel unwell and tired, and may affect your ability to drive. Read more about driving with diabetes.
Always ask your doctor or pharmacist if your medicines are likely to affect your driving. Check this list of high risk medicines(external link) that under Aotearoa New Zealand law, you could be penalised for if you're over the specific blood limit for that medicine.
Some types of medicines known to affect driving include:
- sleeping pills, benzodiazepines and zopiclone
- some antidepressants and antipsychotics
- some pain relievers
- some medicines for epilepsy
- some heart medicines
- some medicines for diabetes
- some medicines for your eyes
- some antihistamines for allergies
- cold and flu medicines
- medicines for nausea and vertigo
- diet pills, 'stay awake' drugs and other medicines containing stimulants (eg, caffeine).
Note: Different combinations of medicines and health conditions can affect people differently.
Video – learn if you are safe to drive when taking any medicines.
(NZTA, 2018)
It's important not to drive until you know how your medicine affects you. Some medicines only have short-term effects when you first start taking them or when you change the dose. This means you might only need to stop driving for a few days until your body adjusts.
However, for other medicines you need to stop driving while you are taking them. Learn to know how your body reacts to the medicines and supplements you are taking. Keep track of how you feel and when the effects occur. Do not drive if your medicine affects you. Check how you feel before getting into your vehicle.
Mixing is when you take more than 1 substance, such as medicines, illegal drugs and alcohol at the same time. Medicines can be prescribed medicines, medicines you might buy over the counter (OTC) in a pharmacy, and other substances with potential medicinal properties related to traditional healing.
Sometimes people take many medicines or illegal drugs, with or without alcohol. This mix, with or without alcohol, makes it far more likely that you will be impaired, making it unsafe for you to drive.
The most common form of mixing is when alcohol is mixed with medicines. Mixing alcohol with illegal drugs and medication can increase your risk of a fatal crash by 23 times.
Alcohol can affect your coordination, reaction time, sleepiness and more. Even though you might be under the legal alcohol limit, you might still be affected and unable to drive.
What you can do
- Always tell your healthcare provider what medicines, including traditional treatments, you are already taking so that they can correctly assess the chances of you becoming impaired.
- Always tell your healthcare provider if you drink alcohol or take illegal drugs, so that they can correctly assess the chances of you becoming impaired.
In March 2023, changes were made to the drug driving legislation in New Zealand with the aim of increasing road safety and reducing accidents caused by drug-impaired driving. There are a wider range of drugs, including some common medicines, that have the highest risk of affecting the ability to drive safely, with new limits and harsher penalties. Read more about the changes to the New Zealand drug driving legislation(external link).
If you're taking medicines that affect your driving, talk to the people you live with about how they could share the driving.
Think about the following scenarios:
- Have a plan for emergencies or unplanned trips. How will you get to an after hours clinic or the hospital if you're unable to drive?
- Have a plan for any change in routine. If you take sleeping tablets at night, what will you do differently if you need to drive late at night or very early the next morning? Or if you take your medication with dinner, what will you do differently if you’re planning to meet friends after dinner in the next suburb?
- Plan your alternatives to driving. Could you share a ride with neighbours or workmates, work from home, take the bus or get a lift with friends? Could you delay your trip to another time of day or to another day?
Medicines that usually cause drowsiness and changes in concentration effect older people more because of age-related changes in the way your body breaks down medicines. This is of concern because older people often take several medicines to stay well, including some that may affect driving. Combinations of medicines can cause more side effects.
All professional drivers in the heavy transport sector need to be aware of the effect of any medication you are taking. The following is a series of videos by NZTA for professional drivers who are taking medicines.
What's the issue?
(NZ Transport Agency, 2019)
Practical tips for drivers
(NZ Transport Agency, 2019)
Practical tips for leaders
(NZ Transport Agency, 2019)
Medication and illegal drugs(external link) Waka Kotahi, NZ Transport Agency
Older drivers(external link) National Institute on Aging, US
References
- Driving rules and assessment for older people(external link) BPAC, NZ, 2010
- Drugs and driving(external link) NZ Formulary
- Medicines can impair driving(external link) Medsafe Prescriber Update, NZ, 2016
- How to show that you are medically fit(external link) Waka Kotahi, NZ Transport Agency
Brochures

Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Stephanie Yee, Pharmacist, Auckland.
Last reviewed:





