Chickenpox vaccine
Also called varicella vaccine
Key points about chickenpox vaccine
- Chickenpox vaccine protects against infection from the varicella zoster virus, which causes chickenpox infection.
- The chickenpox vaccine is also called Varilrix®.
- Find out about the vaccine and possible side effects.

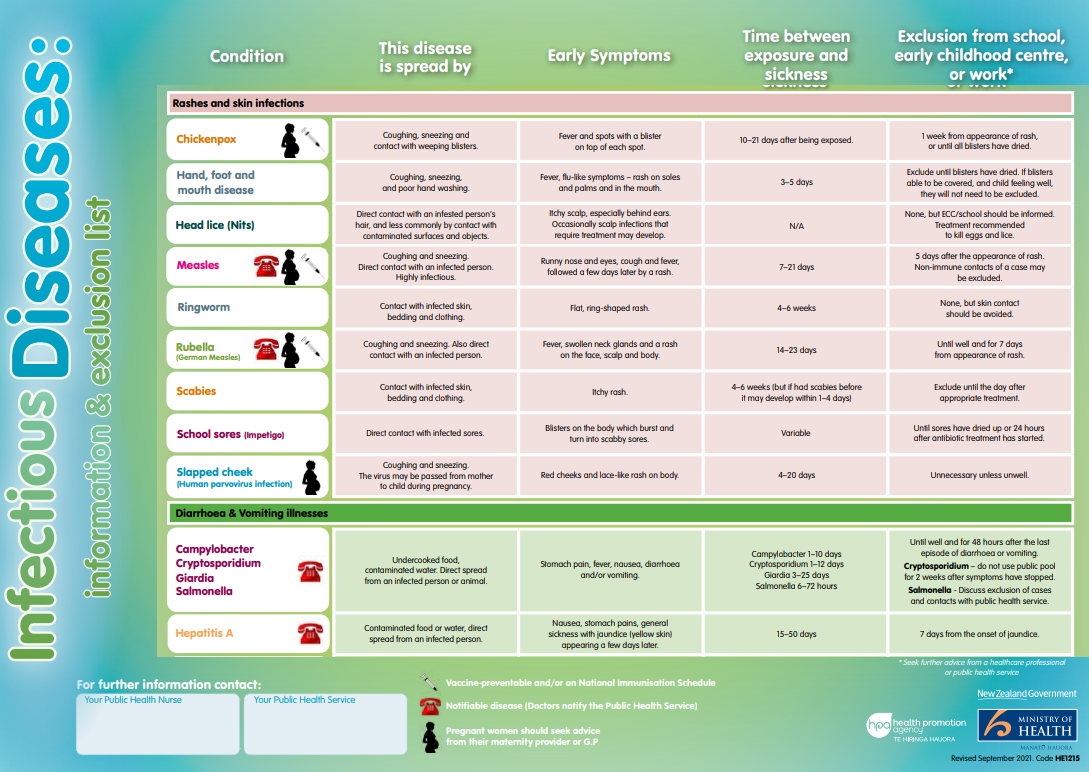
The chickenpox vaccine protects against infection from the varicella zoster virus, which causes chickenpox infection. The virus is easily spread by sneezing and coughing, or by contact with weeping chickenpox blisters. You can even catch the chickenpox virus from touching clothing or other objects that have fluid from the blister on them.
The chickenpox vaccine is a live vaccine which is made using chickenpox viruses that have been weakened (or attenuated), before being included in the vaccine. After vaccination, the weakened vaccine viruses replicate (grow) inside you. This means a very small dose of virus is given to stimulate a response by your immune system.
Live attenuated vaccines don't usually cause disease in vaccinated people who have a healthy immune system. When a live attenuated vaccine does cause any illness, it's usually milder than if you had caught the disease. Live attenuated vaccines given by injection are generally effective after 1 dose.
Video: Chickenpox – disease and vaccine, New Zealand
(The Immunisation Advisory Centre, NZ)
For most people, chickenpox is a mild disease that doesn't cause any lasting problems. About 1 in 20 healthy children develop a bacterial skin infection from chickenpox, which needs antibiotic medicine. If they're not treated, bacterial skin infections can lead to bacterial infection in other parts of your body, including pneumonia and blood stream infection (septicaemia). Other complications of chickenpox are rare and include encephalitis (brain inflammation) and inflammation of your joints, kidneys and liver.
Chickenpox tends to be more severe in adolescents and adults, pregnant women and their unborn babies and people of any age with poorly functioning immune systems. Read more about chickenpox.
If you’re pregnant or planning a pregnancy
If you’re pregnant and get infected with chickenpox the virus can spread to your baby. The highest risk is during the first 20 weeks of pregnancy.
In unborn babies who are exposed to chickenpox through the mother, up to 2 in 100 are born with congenital varicella syndrome. They may have skin scarring, eye, limb and brain abnormalities, developmental delay, and a poor outcome.
If a newborn baby gets infected with chickenpox, up to 30 in 100 will develop severe disease that can result in death.
Pregnant women shouldn't be given the chickenpox vaccine because it's safety for the unborn baby hasn't been tested. However, no harmful effects have happened when pregnant women have been given the vaccine.
Women who are planning a pregnancy and have never been infected with or vaccinated against chickenpox need to be immunised against chickenpox. After you get vaccinated, you should avoid getting pregnant for at least 1 month.
Chickenpox vaccination is recommended and funded in Aotearoa New Zealand for the following groups:
- Children turning 15 months of age
- Children turning 11 years of age who have never been infected with or previously vaccinated against chickenpox.
The vaccine is funded for certain high-risk individuals and/or their close contacts, regardless of age. People with a weakened immune system are at high risk, but may not be able to have the vaccination themselves, so it's recommended that close contacts of these people be vaccinated. Discuss this with your healthcare provider.
Chickenpox vaccination is also recommended, but not funded, for:
- teenagers and adults who have never been infected with or vaccinated against chickenpox
- women who are planning a pregnancy and have never been infected with or vaccinated against chickenpox (eg, those born and raised in tropical countries)
- people who aren't immune to chickenpox and who are working in professions where they come into contact with young children
- parents who haven't had chickenpox.
Chickenpox vaccine is a live vaccine. This means that it can cause chickenpox, although it is usually milder, and it shouldn't be used for certain groups of people who have reduced infection-fighting ability (immunity). This includes people who:
- are pregnant (pregnancy should be avoided for 4 weeks following vaccination)
- are taking high-dose oral steroids (eg, prednisone or dexamethasone)
- are getting chemotherapy or radiation
- have a condition that reduces immunity (eg, cancer or HIV)
- have active untreated TB (tuberculosis)
- have had another live vaccine (eg, MMR, BCG) within the past 4 weeks.
A single chickenpox vaccine dose provides about 99% protection against severe disease and 80% protection against chickenpox infection at all. It's still possible to get chickenpox after having the vaccine, but the infection is usually mild.
The chickenpox vaccine is given as an intramuscular injection (injected into the muscle either in your thigh or upper arm). It's usually given as 1 dose, but 2 doses may be recommended for some people.
The chickenpox vaccine can be administered with some other vaccines, including MMR, at different injection sites. If the chickenpox vaccine isn't given at the same visit as another live injectable vaccine such as MMR, they should be separated by 4 weeks or more.
Like all medicines vaccines can cause side effects, although not everyone gets them.
| Side effects | What should I do? |
|---|---|
|
Read more: After your immunisation.(external link) |
|
Read more: After your immunisation.(external link) |
|
Read more: After your immunisation.(external link) |
|
|
Read more about medicines and side effects and reporting a reaction that you think might be a side effect.
There are many different settings in which you can get a vaccination. These include medical or health centres, pharmacies, community-based clinics including marae-based clinics, mobile health clinics and mobile vaccination services.
Read more about who can give vaccinations and where to get vaccinated.
Vaccines on the National Immunisation Schedule(external link) are free. Other vaccines are funded only for people at particular risk of disease. You can choose to pay for vaccines that you aren't eligible to receive for free.
The following links have more information on chickenpox vaccines:
Chickenpox (Varicella)(external link) The Immunisation Advisory Centre, NZ
Tips following immunisation(external link) Health New Zealand | Te Whatu Ora
Resources
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ English(external link), te reo Māori(external link)
References
- Varicella (chickenpox)(external link) Immunisation Handbook, NZ, 2020
- Varicella (chickenpox)(external link) The Immunisation Advisory Centre, NZ
- Varilrix(external link) The Immunisation Advisory Centre, NZ
Brochures
HealthEd, NZ, 2020
Te reo Māori
HealthEd, NZ, 2023

Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





