If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Eating disorders
Key points about eating disorders
- An eating disorder is an overall term for a number of conditions that involve difficulties with eating. They can be due to a range of factors including managing emotions, and feelings about body weight, shape and food.
- The most common eating disorders are anorexia, bulimia and binge eating disorder.
- Eating disorders have significant effects on mental health, physical health, wellbeing and social functioning.
- The causes of eating disorders are complex and don't involve just one factor.
- Treatment of an eating disorder is very important and can be effective, particularly if offered as early as possible. With treatment, most people make a good recovery, but it may take several years.

An eating disorder is one of a number of conditions that involve disordered eating patterns. The person affected tends to be focused on their weight and body shape. Eating disorders can affect all genders, but can be more common among young adult females.
Anorexia nervosa involves severe dietary restriction, weight loss, loss of menses (menstrual periods) in women, and sometimes purging behaviour (eg, vomiting, using laxatives, excessive exercise).
Bulimia nervosa involves regularly binge eating food in an uncontrollable way and purging to compensate for the eating and fear of weight gain.
Binge eating disorder involves regularly binge eating without purging and is the most common eating disorder.
A newer category of eating difficulties is avoidant restrictive food intake disorder (ARFID). This is different from other eating disorders as it involves a disinterest in food for reasons other than a preoccupation with weight and shape.
There are lots of myths about eating disorders, here are some:
- Myth # 1: You can tell by looking at someone that they have an eating disorder.
- Myth # 2: Families are to blame.
- Myth # 3: Mothers are to blame.
- Myth # 4: Eating disorders are a choice.
- Myth # 5: Eating disorders are the province of white upper-middle class teenage girls.
- Myth # 6: Eating disorders are benign.
- Myth # 7: Society alone is to blame.
- Myth # 8: Genes are destiny.
- Myth #9: Eating disorders are for life.
Disordered eating and eating disorders are related as they are both about having problematic eating patterns. Disordered eating refers to when you no longer have the usual habits of eating that most people have. This can affect how often you eat, how much you eat, the type of food you eat, how flexible you are around your eating habits and whether you experience pleasure in eating. Depending on the eating disorder, it may involve severe avoidance of eating or purging (getting rid of) food you have eaten.
Many people may not meet all the diagnostic criteria for a particular diagnosis, but have extreme distress and difficulties with their eating and self-concept.
‘Orthorexia’ is a term that's sometimes used to describe a concern about the quality of food ingredients and a focus on eating foods that are considered ‘healthy’ or ‘pure’. This preoccupation with eating can also lead to psychological difficulties.
If you no longer have a sense of what is normal eating, you can read about healthy eating basics.
Eating disorders happen because of a combination of factors.
These factors can be:
- biological (the way your brain works)
- genetic (things you inherit)
- psychological (how you think)
- social (your relationships with other people)
- cultural (the customs and values of the people around you),
- societal (messages you get about your body shape and size).
Other factors include responses to trauma and issues related to gender identity.
Eating disorders can affect any age or gender; however, women are more often affected, particularly younger women.
Anorexia and bulimia can develop at any stage in life, but most often occur during adolescence and early adulthood. Binge eating disorder can occur at any time, but can often start in mid-adulthood. Avoidant restrictive food intake disorder (ARFID) is likely to start in childhood. Any of these disorders can have a serious impact on your health.
People at risk of an eating disorder have often experienced the following:
Self-care and getting support from others is vital in recovering from an eating disorder and feeling happy again. If eating disorders are not treated, they can result in serious medical problems, so seek help sooner than later.
Start by talking to your healthcare provider as they can refer you to an eating disorder specialist who understands what you are going through and knows how to help you. Find out more about eating disorder services in Aotearoa New Zealand(external link).
It also helps to learn about your condition. Read more about anorexia, bulimia, binge eating disorder(external link) and avoidant restrictive food intake disorder.
Video: The outlook for someday – disorder
This video is an M-rated intimate insight into the perspectives of people who have lived with disordered eating.
(Day One Hāpai te Haeta, NZ, 2018)
Treatment can help prevent symptoms of disordered eating from progressing to a more severe or chronic state and/or developing into a serious eating disorder. With treatment, many people with an eating disorder make a good recovery, although it may take several years.
If your healthcare provider thinks you most likely have an eating disorder, they will refer you to an eating disorder specialist or service. Most services that treat people with eating disorders bring together a team of different healthcare professionals, including psychiatrists and other doctors, psychologists and dietitians. Some treatment is publicly funded.
Treatment for eating disorders involves normalising eating, together with medical care and psychological treatment. You may need to learn how to manage your feelings in a different way. Some people might also be prescribed medicines.
Most people with eating disorders have mainly outpatient treatment, but you may need to go to hospital for treatment if you are at risk of serious medical problems.
Learning how to take good care of yourself and manage your emotions is key to recovering from an eating disorder. The following steps can help you on your road to recovery.
- Learn about eating disorders to help you make sense of how you feel.
- Seek help early. The longer you leave it, the harder it is to get well.
- Make a decision to recover – see your healthcare provider and get the treatment you need.
- Don’t be so hard on yourself – seek support and learn strategies to help you deal with difficult emotions and thoughts.
- Learn about nutrition and develop a healthy relationship with food.
- Learn ways to improve your body image – self-acceptance and kindness to yourself are important to help you recover.
- Feeling good about yourself is key – make time for pleasurable activities and spend time with people who can boost your mood.

Image credit: Depositphotos
Apps reviewed by Healthify
You may find it useful to look at some Eating disorder apps, Nutrition apps and Mental health and wellbeing apps.
Are you concerned a friend may have an eating disorder? How can you be sure and what can you do or say?
Eating disorders such as anorexia or bulimia are serious medical conditions, which can be fatal if left untreated. If you’re approaching a friend about a suspected eating disorder, remember to do so in a caring, non-judgemental way.
Many people with eating disorders say they are fine and just want everyone to leave them alone. However, in reality, they may be feeling scared and isolated and unsure how to stop the eating disorder from controlling their life. They can put a lot of effort into hiding the condition, so it can be difficult to diagnose. But the earlier a diagnosis is made, the better the chance of recovery.
Here are our top five tips for supporting a friend with an eating disorder.
1. Know your facts
Before you talk to your friend, it's helpful to talk to someone who knows about eating disorders and/or to have read up on the topic. For example, there are different types of eating disorders, symptoms and possible causes.
2. Be kind and non-judgemental
The last thing a person with an eating disorder wants is to feel judged. They may already be feeling alone, confused and ashamed. Knowing they have a friend who cares and who will listen is often the first and most important step in helping them on the road to recovery. Try to use language that isn’t critical or judgemental and be compassionate.
3. Be honest
Being honest about your concerns shows your friend you care. While it may be a conversation you're nervous to have, it’s an important one that may be life-saving. It helps to pick a time and location where you can talk face-to-face in private and your friend is feeling comfortable and relaxed.

Image credit: Canva
4. Encourage them to seek professional help
The most important thing you can do, apart from letting your friend know you’re there to help, is to encourage them to seek professional help. The longer an eating disorder is left untreated, the harder it is on their body and mind to recover. Encourage them to see their healthcare provider, who can provide a diagnosis and advice on where to get further help.
5. Keep supporting them
Be aware your friend may become defensive or angry and even try to deny they have a problem. You can’t force somebody to seek help, especially if they’re an adult, so just keep letting them know you’re there to support them. Once they do seek professional help, keep supporting them throughout their journey to recovery.
6. Support yourself
Everyone needs support, so make sure you have people to support you too.
Remember, if your friend’s health or life is at risk, then seek medical advice immediately.
EDANZ(external link) Help, support and understanding for people with eating disorders and their families
FEAST(external link) For parents of children with eating disorders
Eating Disorders Carer Support (EDCS)(external link) provides support for people caring for people with eating disorders or disordered eating. The also have a Facebook page(external link).
Just a thought(external link) NZ
Togetherall(external link) UK
Eating Disorders Anonymous(external link) US
Disordered eating(external link) Centre for Clinical Interventions, Australia
Atypical anorexia(external link) Centre for Clinical Interventions, Australia
Body image and body dissatisfaction(external link) Centre for Clinical Interventions, Australia
Self help resources for mental health problems(external link) Centre for Clinical Interventions, Australia
Eating disorders(external link) Mental Health Foundation, NZ
Information for parents, caregivers, family and whānau(external link) Tupu Ora Starship Inpatient Eating Disorders Service, NZ
Apps
Eating disorder apps
Mental health and wellbeing apps
Nutrition apps
Brochures
Note: Some of these resources are from overseas so some details may be different. In New Zealand, ring 111 for emergencies, or Healthline 0800 611 116.
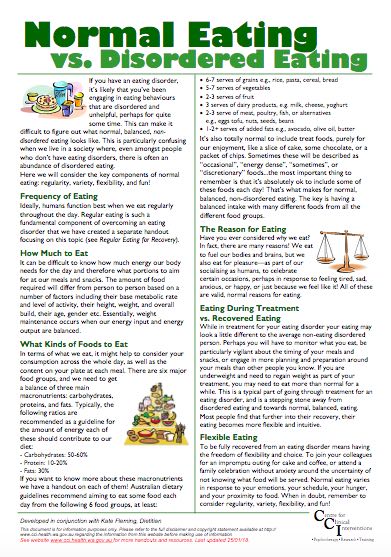
Normal eating vs disordered eating(external link) Centre for Clinical Interventions, Australia
What are eating disorders?(external link) Centre for Clinical Interventions, Australia
Eating disorders – what are the risks?(external link) Centre for Clinical Interventions, Australia
Eating disorders – your guide to what they are and how they are treated(external link) Royal Australia and New Zealand College of Psychiatrists
Family based treatment – information for consumers, carers and professionals(external link) Centre for Clinical Interventions, Australia
Eating disorders(external link) Wharaurau, NZ
Eating disorders – about more than food(external link) National Institute of Mental Health, US
Eating disorders – information for youth(external link) Children’s Hospital of Eastern Ontario, Canada
Tupu Ora – starship inpatient eating disorders service(external link) Starship Children's Hospital, NZ
Body image and body dissatisfaction(external link) Centre for Clinical Interventions, Australia
He rongoā kei te kōrero – talking therapies for Māori(external link) Te Pou, NZ
Talking therapies for Asian people(external link) Te Pou, NZ
Talking therapies for Pasifika peoples(external link) Te Pou, NZ,
References
- Eating disorders(external link) Royal Australian & NZ College of Psychiatrists, 2024
- Normal eating vs disordered eating(external link) Centre for Clinical Interventions, Australia, 2018
- Feng B, Harms J, Chen E, et al. Current discoveries and future implications of eating disorders(external link) Int J Environ Res Public Health 2023;20(14):6325
- Heruc G, Hurst K, Casey A, et al. ANZAED eating disorder treatment principles and general clinical practice and training standards 2020(external link) J Eat Disord. 2020;8(63)
Clinical guidelines
Hay P, Chinn D, Forbes D, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders(external link) Aust N Z J Psychiatry 2014;48:977–1008
Managing frequently encountered mental health problems in young people – non-pharmacological strategies(external link) BPAC, NZ, 2015
Management of eating disorders for people with higher weight – clinical practice guideline(external link) National Eating Disorders Collaboration, Australia
See our page Long-term conditions for healthcare providers
Other resources
Eating disorders | Core skills(external link) for GPs Whāraurau, NZ
Management of eating disorders(external link) Starship Children’s Hospital, NZ, 2021
Eating disorders – recognition and treatment(external link) NICE, UK, 2017
Classifying eating disorders – DSM 5(external link) Eating Disorders Victoria, Australia, 2016
Eating disorder services(external link) Healthpoint, NZ
SCOFF questionnaire The SCOFF Questionnaire is a brief five-question screening tool validated for use in specialist and primary care settings.
Continuing professional development
E-learning
Professional development(external link) National Eating Disorders Collaboration, Australia
Eating disorder core skills – eLearning for GPs(external link) National Eating Disorders Collaboration, Australia
Eating disorders(external link) Goodfellow e-Learning, 2019
Eating disorders – core skills for GPs' e-learning(external link) Whāraurau, NZ
Webinar
Does your patient have an eating disorder?(external link) Goodfellow Unit Webinar, NZ, 2018
Brochures

Centre for Clinical Interventions, Australia, 2018
Centre for Clinical Interventions, Australia, 2018
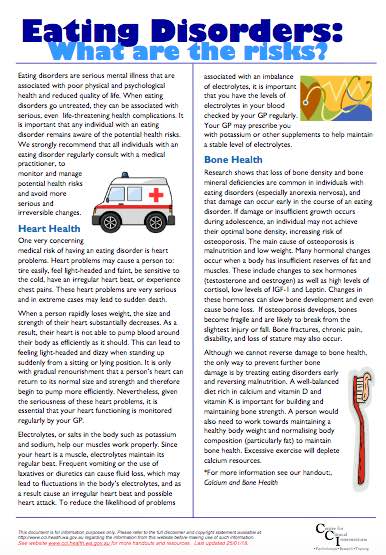
Centre for Clinical Interventions, Australia, 2018
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Michelle Meiklejohn, Clinical psychologist
Last reviewed:





