If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Worms in humans
Key points about worms in humans
- People can get worms in different ways, depending on what type they are.
- Threadworms are the most common type of worm infection in Aotearoa New Zealand. They usually cause an itchy bottom, and sometimes itchy genitals.
- Other worms such as tapeworm, hookworm, roundworm, whipworm and Strongyloidiasis are rare in Aotearoa New Zealand as they can only be picked up overseas. They’re common in countries where sanitation and hygiene are poor.
- Healthify has a separate page on threadworms, this page covers the other types of intestinal worms.

Overview
People can get worms in different ways, depending on what type they are. Worms are called parasites because they live in a host, such as humans or pets, and get nourishment and other needs from the host. Most people get worms by accidentally swallowing them or their eggs. Most worm infections are not serious and can easily be treated with medicine.
- Threadworms are the most common worm infection in Aotearoa New Zealand. Threadworms commonly cause an itch around the bottom and genitals. Read more about threadworms.
- Other worms such as tapeworm, hookworm, whipworm and Strongyloidiasis are rare in Aotearoa New Zealand as they can only be picked up overseas. They're common in countries where sanitation and hygiene are poor. Read more about tapeworm, whipworm, hookworm and Strongyloidiasis below.
- Most worm infections are treated with the worm medicine mebendazole. Tapeworm is treated with praziquantel. Your healthcare provider will advise you on the best treatment for you.
Tapeworms are rare in Aotearoa New Zealand. They're common in countries with poor sanitation and hygiene.
The word 'tapeworm' describes the flat shape of the worm, like a tape measure ribbon or like long flat pasta such as tagliatelle.
- Tapeworms can come from a variety of different animals, but mostly from cows and pigs.
- People usually become infected by eating undercooked beef or pork. If it contains tapeworm larvae it's called 'measly' and if you eat a cyst you'll get a worm.
- If you eat pork that contaminated with tapeworm eggs you can get a more serious illness called 'cystercicosis'.
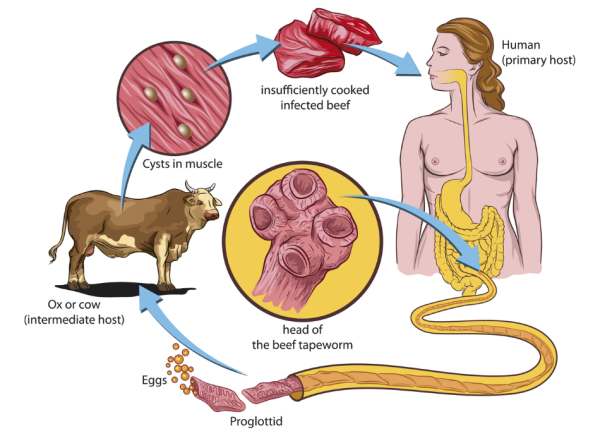 Image credit: Depositphotos
Image credit: Depositphotos
Symptoms
Most tapeworms don't cause symptoms. You may only find out you have a tapeworm if you notice a bit of worm in your poo. The pieces of worm may move about, which can seem disgusting but isn't dangerous. The most common tapeworm pieces are 1 to 2 cm long, but they may be much longer if lots of pieces are joined together. Sometimes the whole tapeworm comes out of your bottom, and then it can be several metres long. Tapeworms are flat and rectangular and white or pale yellow in colour.
Diagnosis
Your healthcare provider can take a stool (poo) sample and examine it for tapeworm eggs under a microscope. If you see a worm in your poo, it can help if you put the poo in a clean container and take it to your healthcare provider. They can send it to a laboratory to find out what it is.
Treatment
Tapeworms are treated with praziquantel tablets. It paralyses and kills the worms and they're then passed out in your poo.
Complications
In rare cases, tapeworms can cause serious problems. This is most commonly due to the pork tapeworm eggs, which can form small fluid-filled cysts in different parts of your body, including your brain. This condition is called ‘cystercicosis’ and is caused by eating food contaminated with the pork tapeworm eggs in other parts of the world.
Whipworms are rare in Aotearoa New Zealand, however they are common in countries where there is poor sanitation and hygiene. .
The name 'whipworm' comes from the worm's whip-like shape.
- People get whipworms by consuming infective eggs found in contaminated soil, if food items aren't carefully washed, peeled and cooked.
- When the eggs hatch inside the bowel (large intestine), the whipworm sticks inside the wall of the large intestine and the eggs are passed out through the poo.
Symptoms
Most people who have a light whipworm infection (only a few worms), don't have symptoms. If there is a heavy infection (many worms), symptoms may include severe frequent, painful poos (diarrhoea) that contain a mixture of mucus, water, and blood, and iron-deficiency anaemia. Heavy infections are more common in children.
Diagnosis
Your healthcare provider can take a stool (poo) sample and examine it for whipworm eggs under a microscope. This is the only way to know if you have a whipworm infection.
Treatment
Whipworm is mainly treated with the worm medicine mebendazole.
Complications
If left untreated, heavy infections can cause problems – mainly in children. Problems include severe anaemia and slow growth.
Hookworms are also rare in Aotearoa New Zealand. As with tapeworms and whipworms, they're common in countries without good hygiene and sanitation.
The name 'hookworm' comes from the hook-like shape of the head of the worm.
- People get hookworm infection by walking barefoot on soil contaminated with hookworm.
- The larvae (immature form of the worm) enter the skin. They then move to the lungs through the bloodstream and enter the airways. The worms are about one centimetre long.
- After traveling up the airways, the larvae are swallowed and infect the gut (small intestine).
- They develop into adult worms and live there for 1 or more years.
- Adult worms and larvae are released in poo.
Symptoms
Symptoms may include stomach pain, abdominal discomfort, cough, runny poo, fever, bloating and gas, itchy rash, loss of appetite, nausea, vomiting and signs of anaemia such as feeling very tired (fatigue) and pale skin.
Diagnosis
Your healthcare provider can take a stool (poo) sample and examine it for hookworms under a microscope.
Treatment
Hookworms are mainly treated with the worm medicine mebendazole.
Complications
If left untreated, a hookworm infection can cause anaemia and nutrient deficiency, mainly protein, caused by blood loss. These effects are more common in children. Blood loss happens because the adult worms attach to your gut and feed on blood. When children are continuously infected by many worms, the protein deficiency and the loss of iron due to anaemia can slow their growth and mental development.
Roundworms (ascaris lumbricoides) are the most common intestinal worm around the world – especially in tropical and subtropical regions. Infections (ascariasis) are most often picked up when travelling overseas.
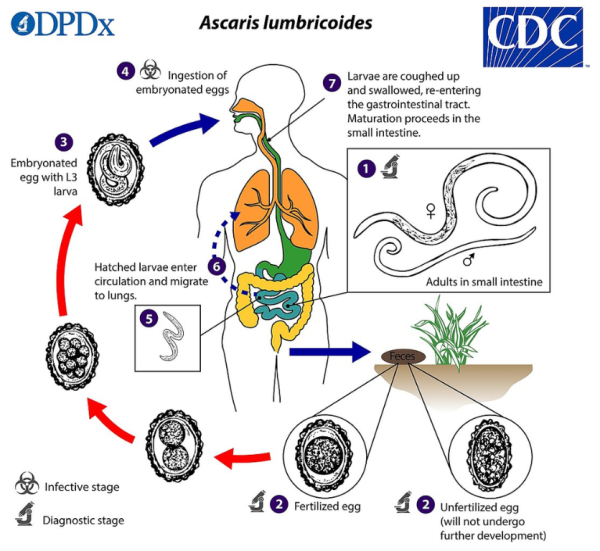
Image credit: Centers for Disease Control via Wikimedia Commons(external link)
The name 'roundworm' comes from the shape of the worm which has a long, unsegmented body and looks like an earthworm.
- People get infected by eating soil that contains roundworm eggs. The contaminated soil is generally found in countries where people defecate (poo) outside, or use human faeces (poo) as a fertiliser.
- The eggs pass from the poo into the ground. They’re then picked up by eating badly washed fruits and vegetables or by handling them and not washing your hands properly.
- The fertilised eggs hatch into larvae (immature form of the worm) which get into the lining of the intestine and then travel to the lungs.
- After traveling up the airways, by being coughed up, the larvae are swallowed and infect the gut (small intestine).
- They develop into adult worms which can live for 1 to 2 years and grow up to 30 cm (male) and 35 cm (female) long.
- Adult worms and eggs are released in poo.
- Humans and pigs are the main hosts.
Symptoms
There may be few or no symptoms with an ascariasis infection, seeing a worm in poo might be the first sign. However, symptoms can include tummy discomfort or pain, diarrhoea, and coughing – due to the movement of the worms through the body. If the infection is bad, you might vomit and lose weight. Also, worms or eggs might be found in the nose or mouth.
Diagnosis
Your healthcare provider can take a stool (poo) sample and examine it for roundworm eggs under a microscope. If you pass a worm in your poo, or cough one up, you can take it in to be identified by your healthcare provider.
Treatment
Roundworms can be treated very well with mebendazole which is available as a flavoured tablet, liquid or chocolate square. Read more about mebendazole.
Complications
If left untreated the worms can migrate to the liver and cause damage. An ongoing severe infection can lead to the gut becoming blocked with worms causing nutritional problems which can affect children’s growth.
Strongyloidiasis (pronounced strong-a-loyd-eye-a-sis) is rare in Aotearoa New Zealand. It's common in countries where sanitation and hygiene are poor.
- You can get Strongyloidiasis by walking barefoot on soil contaminated with it.
- The larvae burrow through your skin and make their way to your lungs, through your bloodstream.
- After traveling up the airways, the larvae are swallowed and infect your gut where they become adult worms.
- These worms then produce eggs that hatch and develop into infective larvae which pass in poo. Some may mature and re-infect your body by digging into the walls of your intestine or anus.
- If you don't get treatment, Strongyloidiasis can last for your whole life but it may not make you feel unwell at all.
Symptoms
Many people infected don’t have any symptoms. Some people may get:
- an itchy rash when the larvae are burrowing under your skin
- chest symptoms such as wheezing and coughing when the larvae reach your lungs
- gut symptoms such as abdominal pain, runny poos and bloating
- nausea, vomiting, weight loss, weakness or constipation.
Diagnosis
Your healthcare provider can identify a Strongyloides infection with a blood test or by using a microscope to look for the larvae in a sample of your poo.
Treatment
Strongyloidiasis is mainly treated with ivermectin.
Complications
Hyperinfection is a rare, but serious, complication of Strongyloides infection. A hyperinfection is where you continue to be re-infected because you have worms and larvae of all stages in your body and their lifecycle keeps going. It's more common if you have a weakened immune system, especially if you're taking prednisone. Hyperinfection can make you very sick and needs to be treated in hospital.
References
- Tapeworm infection(external link) DermNet, NZ, 2013
- About human tapeworm(external link) CDC, US, 2024
- Hookworm infections(external link) DermNet, NZ, 2013
- About hookworm(external link) CDC, US, 2024
- Trichuriasis (whipworm)(external link) DermNet, NZ, 2013
- About whipworms(external link) CDC, US, 2024
- Strongyloidiasis(external link) DermNet, NZ, 2008
- About Strongyloides(external link) CDC, US, 2024
- Anthelmintics(external link) New Zealand Formulary
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Tim Cutfield, Infectious Diseases and General Physician, Auckland
Last reviewed:





