Trigeminal neuralgia is pain felt in the side of your face (jaw, cheek or teeth). The pain can vary from being sharp and stabbing to dull and achy and can arrive suddenly and last for a few seconds or minutes before stopping. There may be a short or long space of time between attacks.
The pain is associated with the trigeminal nerve (fifth cranial nerve) which is one of the main nerves connecting your brain and your face. There’s one on each side of your face.
The trigeminal nerves transmit pain and touch signals from your face to your brain and control your jaw's muscle movements and the production of saliva and tears.
Each trigeminal nerve has 3 small branches:
- First or ophthalmic branch – this supplies your scalp, forehead and around your eye.
- Second or maxillary branch – this supplies your cheek.
- Third or mandibular branch – this supplies the area around your jaw.
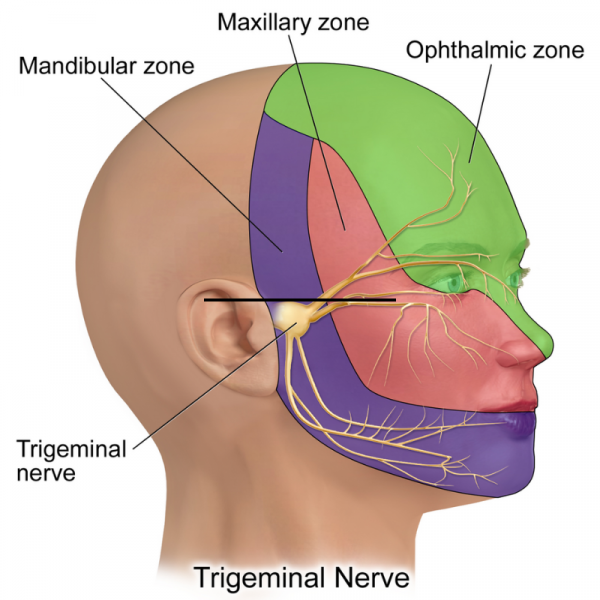
Image credit: BruceBlaus via Wikimedia Commons(external link)






