Staph skin infections – recurring
And how to stop them
Key points about recurring staph infections
- Staphylococcus aureus (or ‘staph’) is a kind of germ (bacteria) that is a common cause of skin infections.
- Most staph skin infections clear up after treatment and seldom return, but for some people staph skin infections can return or be an ongoing problem.
- Recurrent staph infections are more common if you have other skin conditions which cause broken skin, such as eczema and dermatitis. Treating the underlying skin condition is the best way to prevent recurrent staph infections.

Staphylococcus aureus (or ‘staph’) is a kind of germ (bacteria) that is a common cause of skin infections such as boils, abscesses, school sores (impetigo) and cellulitis. Staph commonly lives on the skin but it will only cause an infection when it can enter through a wound or open skin. Learn more about staph skin infections.
Most staph skin infections clear up after treatment and seldom return, but for some people staph skin infections can recur (come back again) or be an ongoing problem.
Recurrent staph infections are more common if you have broken skin from other skin conditions such as eczema and dermatitis. Treating the underlying skin condition is the best way to prevent recurrent staph infections.
There are other things you can do to prevent recurrent staph infections such as:
It's also important to keep your household clean to prevent recurrent skin infections. Staph bacteria can survive on towels, bedding, doorknobs, countertops, and shared items. Regular cleaning and disinfecting reduces the number of germs that could come into contact with your skin. Read more about good hygiene in your home.
Make sure you treat other skin conditions. If you have skin conditions such as eczema, psoriasis, or a fungal infection such as athlete's foot, it’s important that these are treated. These skin conditions damage your skin’s protective barrier, leading to small cracks or open areas, which make it easier for staph bacteria to cause infection.
Minor wounds or small infections (smaller than a 10 cent piece) can be treated with an antiseptic (eg Crystaderm, Savlon, Betadine). Always cover infections with a plaster to stop them spreading.
If you have any signs of more serious infection, such as pain and spreading redness of your skin or fever, contact your healthcare provider to get these treated as soon as possible.
It’s also important to avoid cuts, grazes or anything that may damage your skin, including tattoos. Damaged skin puts you at risk of recurrent infection.
- Keep the sore or infected area covered with a dressing or plaster until it has healed up. Don’t scratch the area and avoid touching it. Wash your hands well after touching the infected area. Antiseptic creams can be used for small cuts and grazes.
- Shaving with a blade can damage hair follicles under the arms, on the legs, and on the face and cause pimples or folliculitis. Electric razors may be better or consider not removing the hair.
- Make sure that your clothing or belt isn't tight and repeatedly rubbing against your skin, such as your thighs, stomach area (abdomen), or buttocks. The constant rubbing or friction can irritate and damage your skin.
It’s important to keep your skin moisturised because when skin becomes very dry, it can crack, flake, or peel. These small breaks create openings where bacteria can enter and cause infection. Dry skin also often leads to itching. If you scratch it, you can damage your skin further, and introduce bacteria from your nails and the environment.
Moisturise your skin at least twice a day if you have eczema or dry skin. Moisturiser is best applied by dotting the product onto your skin and then spreading it using a downward stroking motion in the direction of hair growth to avoid blocking hair follicles. It's not necessary to rub the product up and down until it's all absorbed. Read more about emollients and moisturisers.
Use steroid creams or ointments for treating eczema as recommended by your healthcare provider.
Use a spoon or spatula to transfer creams into smaller containers to prevent contamination. If you think the cream has become contaminated, throw it away.
Bathe or shower with lukewarm water and use products that are fragrance-free, alcohol-free, and non-irritating. Avoid harsh or abrasive soaps and very hot water because these can remove the skin’s natural oils and cause dry, irritated, or cracked skin.
If you or anyone in your house has an infected cut or sore, cover it with a plaster. This will help stop it infecting other parts of your body and stop it spreading to other people. Any type of plaster is fine.
Keep your fingernails clean and short and wash your hands properly with liquid soap and water or an alcohol-based hand gel. Make sure you clean between your fingers and up to your wrists.
Take a bath or shower once a day, and more often if you sweat a lot or do physical activities. If your skin is dry and you’re not very active, bathing every second day is usually fine. Make sure to rinse your whole body, including between your toes, under your arms, around your bottom, in your groin area, and in any skin folds.
Don’t share towels, sheets, soaps, clothing, razors, make-up or other personal items. Throw away used razors.
Make sure towels are dry before using them. Wash your towels daily if you have a skin infection. If there is no infection, wash your towels and bed linen once a week. Wash towels and sheets in hot water if you can.
You should also regularly do these things in your home:
- Wash towels and sheets regularly in hot water or add a capful of bleach to the wash cycle. Dry them well before use.
- Clean bench tops, doorknobs, bathtubs and toilet seats often.
- Clean all hard surfaces, including bathrooms and floors, with detergent and water.
- Regularly vacuum carpets, rugs, mattresses and electric blankets.
- Wash pet bedding regularly, especially dog bedding.
- Wash and dry your child’s sports clothing after each match.
The following links provide further information about stopping staph skin infections.
Optimising the skin barrier to infection(external link) Capital & Coast DHB and Hutt Valley DHB
Staphylococcal infections (staph)(external link) Plunket, NZ
Staphylococcal infections(external link) The Royal Children’s Hospital Melbourne, Australia
(external link)
Resources
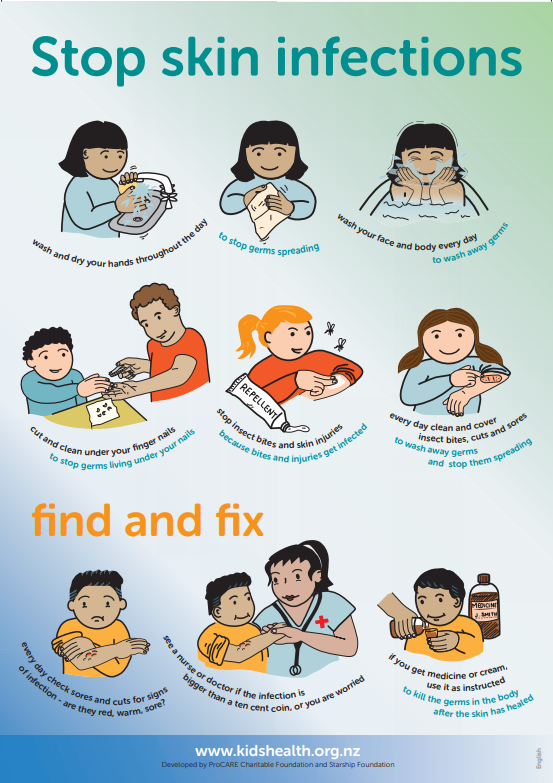
Stop skin infections(external link) Northern Region Skin Prevention Group with support from Health Literacy NZ, KidsHealth, Procare Charitable Foundation and Starship Foundation NZ. Available in the following languages: English(external link), te reo Māori(external link), Samoan(external link), Tongan(external link)
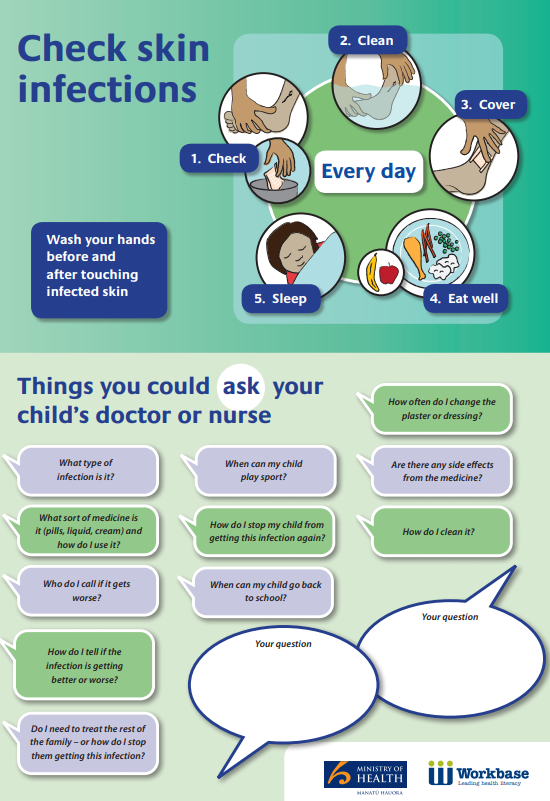
Check skin infections – things you could ask your child's doctor or nurse(external link) Ministry of Health and Workbase NZ
Optimising the Skin Barrier to Infection [PDF, 73 KB] Senior Medical Experts (SMEs) Capital & Coast DHB and Hutt Valley DHB
Preventing & treating staphylococcal skin infections(external link) HealthInfo, NZ, 2018
References
- Bleach baths in patients with skin infections(external link) Dermnet NZ, 2015
- Managing skin infections in Māori and Pacific families(external link) BPAC, NZ, 2012
- Staphylococcal skin infection(external link) DermNet NZ, 2015
Brochures

Optimising the Skin Barrier to Infection
Senior Medical Experts (SMEs) Capital & Coast DHB and Hutt Valley DHB
Northern Region Skin Prevention Group with support from Health Literacy NZ, KidsHealth, Procare Charitable Foundation and Starship Foundation NZ
Available in the following languages:
Te reo Māori
Samoan
Tongan
Ministry of Health and Workbase NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Arna Letica, FRNZCGP, Auckland
Last reviewed:
Page last updated:





