You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Skin infections in children
Key points about skin infections in children
- A skin infection happens when bacteria, fungi or parasites get into your skin and spread.
- They can cause pain, swelling, itch and redness.
- A skin infection may be mild or serious.
- Find out about common types of skin infections children can get and when to take them to see a healthcare provider.

Your skin is the largest organ of your body. One of its functions is to protect your body from infection. Sometimes the skin itself gets infected.
Skin infections are caused by many different types of bacteria, fungi and parasites. These can get into your body through a break in your skin, such as a cut or a scratch. Symptoms can vary from mild to serious.
Skin infections are different from rashes. A rash is an area of inflamed or irritated skin. While rashes can be symptoms of some skin infections, a person with a rash does not necessarily have an infection. Learn more about rashes in children.
Some common skin infections found in children are:
- boils and abscesses
- cellulitis
- school sores (impetigo)
- scabies
- fungal skin infections (tinea or ringworm).
Common breaks in the skin which can lead to infection are:
- cuts, scratches and grazes
- eczema
- insect bites.
A brief summary and a link to learn more is provided below.
Boils and abscesses
These are red bumps or pimples with red skin around the outside caused by a lump of pus under the skin. You may be able to see white or yellow pus through the skin in the middle. It can be sore or itchy. A large boil is called an abscess. Read more about boils.

Image credit: Canva
Cellulitis
Cellulitis (pokenga kiri) is an infection of the deeper layers of the skin. The skin becomes red, painful, hot and swollen. Your child may get a fever and feel very unwell. Cellulitis can spread quickly and it’s important you get medical help straight away. Treating it early with antibiotics can stop the infection getting more serious. Read more about cellulitis.

Image credit: John Campbell via Wikimedia Commons(external link)
Impetigo (school sores)
Impetigo is commonly known as school sores. It’s caused by 2 types of bacteria (strep or staph). It causes skin sores, usually on your hands and face, often around your mouth and nose. Impetigo spreads to other people very easily. It’s important to get treatment from a healthcare provider and keep children away from others to stop the spread. Read more about impetigo (school sores).

Image credit: DermNet NZ(external link)
Scabies
Scabies (waihakihaki) is a contagious skin condition that causes a very itchy rash. The rash is caused by an allergic reaction to a tiny mite that burrows under your skin. It spreads very easily by skin-to-skin contact or touching bedding and clothing of somebody with scabies. It won’t go away by itself and everyone in your household will need to be treated. Read more about scabies.

Image credit: DermNet NZ(external link)
Tinea (fungal skin infections)
These are skin infections caused by a fungus. They’re known by different names depending on which part of your body is affected, such as athlete’s foot and scalp ringworm. With a fungal infection your skin may be red and itchy and may burn or sting. Find out more about the symptoms and treatment for the different types of tinea skin infection.

Image credit: DermNet NZ(external link)
Cuts, scratches and grazes
Broken skin allows bacteria to get through and cause an infection. It’s important to clean, cover and check broken skin and get advice if you see any signs of infection. Learn more about cuts and grazes.
Eczema
Eczema, or atopic dermatitis, is a common skin condition leading to dry, itchy and red skin. Because it’s itchy, children are likely to scratch and break the skin which can lead to an infection. If their eczema looks weepy and crusted, has little pimples or blisters in it, or is very painful or spreading, see your healthcare provider for advice. Read more about eczema in children.

Image credit: DermNet NZ(external link)
Insect bites
After an insect bite you can get a raised red bump, possibly with a blister in the middle. It can be itchy or sore. If the red swollen area keeps getting bigger or more painful, if there is pus or it lasts longer than 2 weeks that could be a sign of infection so seek medical advice. Read more about insect bites.
Take your child to a healthcare provider if they have a sore or wound that:
- is bigger than the size of a 10 cent coin (about 1.5 cm)
- is getting bigger
- has pus
- has red streaks coming from it
- is not getting better after 2 days
- is close to their eye
- won’t stop bleeding.
If skin infections are not treated, they can lead to other serious health problems. Your child may end up in hospital with a serious skin infection or blood poisoning (sepsis) which can hurt their lungs, kidneys and brain.
Treatment depends on the type of infection and how serious it is. Some can be treated with good hygiene (eg, cleaning the area with warm water and covering it with a plaster or bandage) or over-the-counter medicines (eg, antiseptic or anti-fungal creams). Other infections may need medical attention (eg, antibiotics for cellulitis). Find out more on each of the pages linked in the related topics section below.
Brochures
Skin problems in children(external link) Workbase Education Trust and Ministry of Health, NZ, 2013
Looking after your child's skin and treating skin infections(external link) Workbase Education Trust and Ministry of Health, NZ, 2013
Healthy skin(external link) Health Literacy NZ
Bleach bath instructions(external link) Paediatric Society of New Zealand, 2025
Antibiotics for your skin(external link) Choosing Wisely, NZ, 2016
Germs and our skin – four lesson plans for years 2 and 3(external link) Health Literacy NZ
Germs and our skin – four lesson plans for years 5 and 6(external link) Health Literacy NZ
References
- Skin problems in children(external link) Ministry of Health, NZ, 2013
Topical antibiotics for skin infections – when are they appropriate?(external link) BPAC, NZ, 2017
Managing skin infections in Māori and Pacific families(external link) BPJ Article, August 2012
Health literacy and the prevention and management of skin infections(external link) Health Literacy NZ
The booklet Looking after your child's skin and treating skin infections(external link) has accompanying guides suitable for health improvement practitioners or kaiawhina:
Talking points for health professionals – first diagnosis(external link) Health Literacy NZ
Talking points for health professionals – follow-up visit(external link) Health Literacy NZ
Talking points for health professionals – preventing infections(external link) Health Literacy NZ
Brochures
Workbase Education Trust and Ministry of Health, NZ, 2013

Workbase Education Trust and Ministry of Health, NZ, 2013
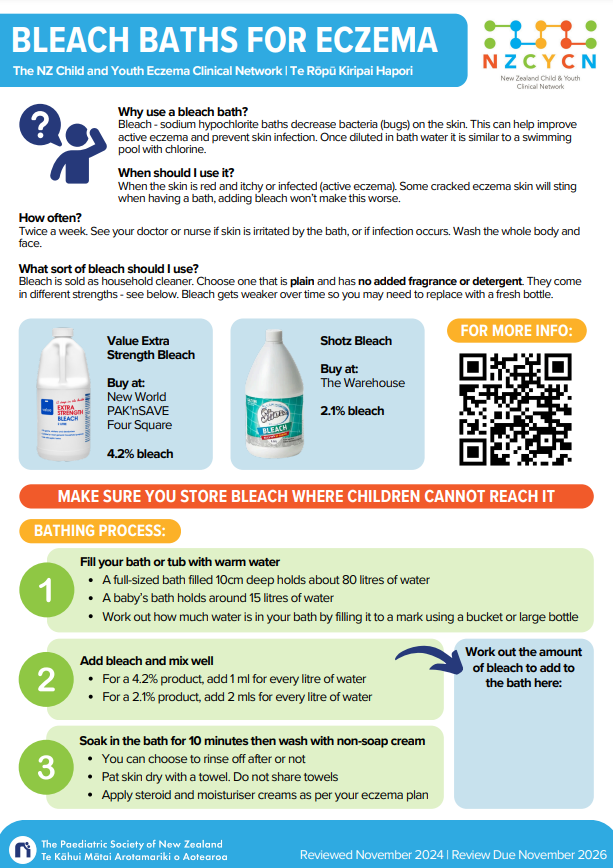
Paediatric Society of New Zealand, 2025
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





