A course of external radiation treatment is given over several days or weeks. Each treatment is known as a ‘fraction’. Fractions may be given every day from Monday to Friday or only 3 days a week. The rest days between treatments give your normal cells a chance to recover.
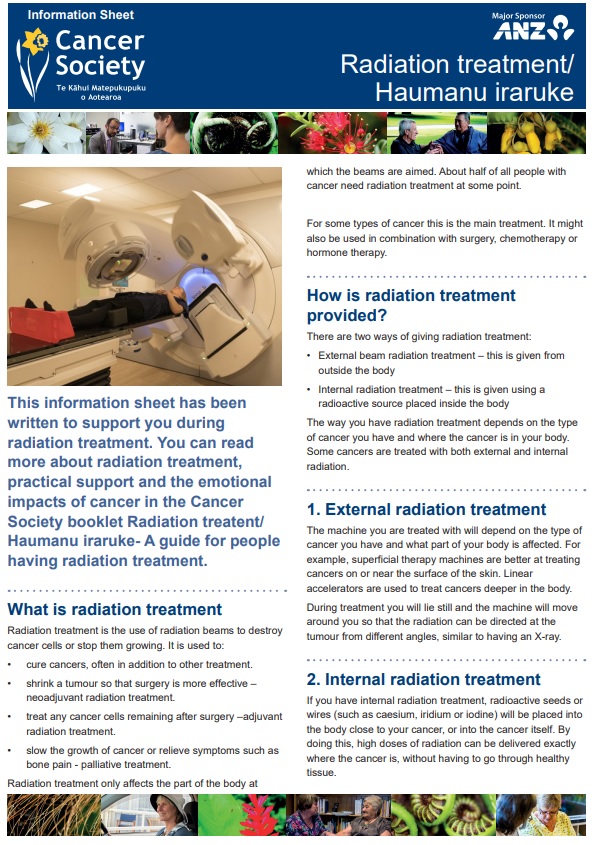
External radiation delivers a beam of radiation using a treatment machine called a linear accelerator. The exact machine used for you depends on the type of cancer you have and where in your body it is.
While you lie still, the machines are moved up and down and around you so that the radiation can be directed at the tumour from different angles. It's similar to having an X-ray taken. During this treatment you don't see or feel anything.
Planning your treatment
The process of planning external beam radiation treatment is complex and might take several weeks to complete. It's a very important part of your treatment because the treatment plan will be designed just for you to give the required dose of radiation to the cancer while sparing as much normal tissue as possible. After your planning session, check with staff on how long it will be before your treatment starts.
Simulation part of planning process
Before you start a course of external radiation treatment you will require at least 1 visit to the cancer centre to work out the exact position you will lie in during your treatment (a simulation). A simulator – a machine similar to a treatment machine or a CT scanner – is used for this.
During planning, the treatment team considers many factors, including:
- what type of radiation to use
- the size and shape of the radiation field
- your position as well as machine positioning
- how much radiation is to be delivered for each treatment
- how many beams of radiation will be used.
This is all done on computers using the information from your simulation, a CT scan, and other tests you have had.
This simulation process can take 30–60 minutes and is a much longer process than each individual treatment. It's important that you lie still in the same position when you have your treatment. You might have a range of supports to help you keep still.
Once the position of the beam is worked out, your skin or the mask (if you need one to hold your head still) will be marked. This may require a tattoo which is a permanent marking, but occasionally can be removed later. It can be helpful to have whānau or a friend with you during simulation and planning.
How long is a course of treatment?
External radiation is usually given in a number of treatments (or fractions). The number of treatments isn't necessarily related to the seriousness of the cancer. It depends on several factors, including your general health, and the site and type of cancer being treated. You might want to allow time before and after treatment each day, as delays in your appointment might occur.
If a high dose of radiation is required, it's usually given on 4 or 5 days a week for 5 to 7 weeks. If a quick response is required (eg, to relieve a cough or pain, stop bleeding or reduce swelling) a shorter course is more likely to be given. The total amount of time spent in the treatment room is usually 10–20 minutes. The machine is only turned on after the therapists have made sure you're in the correct position.
The actual treatment usually takes a very short time – a few minutes at most. Radiation treatment is available in Auckland, Hamilton, Tauranga, Palmerston North, Wellington, Christchurch and Dunedin. External radiation is usually given to you as an out-patient. If you're already in hospital, you'll be taken to the radiation treatment department each time.
Will external radiation make me radioactive?
No. External radiation treatment doesn't make you radioactive. It is safe to be with your children, family and friends both throughout the treatment and after the treatment has been completed.