Video: How a peptic ulcer develops
This video may take a few moments to load.
(Bupa Health UK, 2013)

Low or no data? Visit Zero Data then search for 'Healthify'. Click on our logo to return to our site and browse for free.

This video may take a few moments to load.
(Bupa Health UK, 2013)
The most common symptom or sign of an ulcer is pain in the abdomen. It often starts within a few hours of eating. Other symptoms include:
In some people ulcers may bleed or perforate (make a hole in the stomach or the duodenum so food and bacteria go into the abdomen) or the area around them may become scarred, blocking up the intestines.
You should talk to a healthcare provider if you think you have a peptic ulcer so that you can get some treatment and pain relief.
Call 111 to get urgent medical help if you:
As well as seeking help from a healthcare professional, there are things you can do to care for yourself:
There are two main types of peptic ulcer, named according to their location.
Peptic ulcers can also occur in your oesophagus (the tube that carries food and liquid from your throat to your stomach).
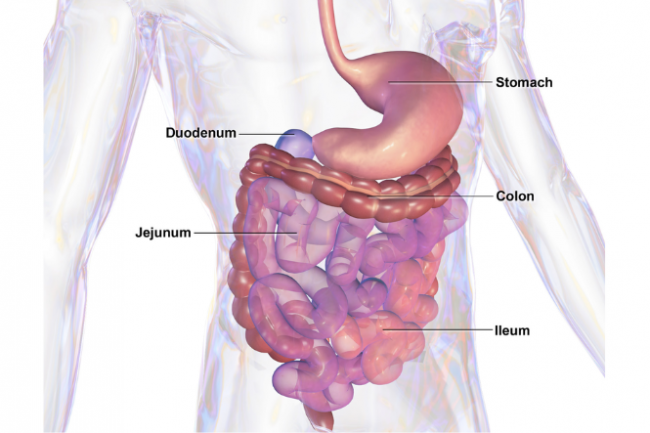
Image credit: blausen.com wikimedia commons
The most common causes of peptic ulcers are bacterial infection and long-term use of non-steroidal anti-inflammatory medicines (NSAID).
Bacterial infection
The majority of peptic ulcers are caused by infection with a bacteria called Helicobacter pylori (H. pylori). Most people with H. pylori infection don't have symptoms of peptic ulcer. The H. pylori bacteria make a substance that damages the mucous lining of the stomach so it can be damaged by acids that break down food during digestion. The bacteria also make the body produce more acid which makes the problem even worse. Read more about H. pylori.
Non-steroidal anti-inflammatory medicines (NSAID)
After H. pylori, the next most common cause of ulcers is taking long term or high dose anti-inflammatory medicines, eg, aspirin, ibuprofen or other non-steroidal anti-inflammatory drugs (NSAIDs). These can work in the same way as a bacterial infection, leaving your stomach open to attack from digestive acids. If you are taking anti-inflammatory drugs long term for pain relief you should talk to your healthcare provider about how you can protect yourself from developing ulcers.
Other causes
See your healthcare provider if you have peptic ulcer symptoms of a peptic ulcer. They may want to test if you have H. pylori infection (with a faecal antigen test or breath test) and you may need further tests such as an X-ray of your stomach and gut or an endoscopy/gastroscopy (to look inside your stomach).
Treatment for your ulcer will depend on what caused it. Medication treatment options include:
With treatment, most ulcers heal in a few months. They can return, but they're less likely to come back if you complete your course of treatment and make appropriate lifestyle changes.
Sometimes peptic ulcers can involve cancer and a repeat gastroscopy may be done to check that the ulcer is healing.
You may find it useful to look at some Digestive health apps and Pain management apps.
The following links provide further information about peptic ulcers. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Stomach ulcers(external link) NHS, UK
Peptic ulcer – a patient's guide(external link) Family Doctor NZ
Peptic ulcers(external link) Auckland Gastroenterology Associates, NZ
Digestive health apps
Pain management apps
Managing dyspepsia and heartburn in general practice – an update(external link) Best Practice Journal (BPJ) and Best Practice Advisory Centre NZ, 2011
H. pylori – who to test and how to treat(external link) BPAC, NZ, 2022
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Derek JY Luo, MBChB (Otago) FRACP, Consultant Gastroenterologist
Last reviewed:
Page last updated: