As well as using self-care methods, there are 2 main types of medicines for treating heartburn:
- Antacids – provide fast relief by lowering the level of acid in your stomach. However, they don’t heal oesophageal damage or prevent heartburn from happening again. Antacids can be bought from a pharmacy. Read more about antacids.
- Proton pump inhibitors – block the stomach making acid which helps to heal any damage in your oesophagus. Examples include omeprazole and lansoprazole. You can buy omeprazole from your pharmacy. Proton pump inhibitors should not be taken for more than 4 to 8 weeks. Read more about proton pump inhibitors.
- Histamine blockers – which reduce the production of stomach acid and help to heal stomach ulcers, eg, famotidine and cimetidine)
If you're pregnant, ask your doctor, nurse or pharmacist to find out whether these medicines are safe for you to take.
Surgery
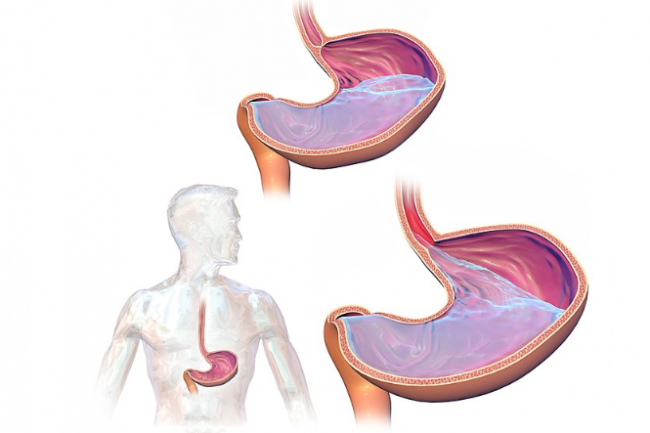
Surgery is an option for a few people with persistent and severe symptoms if lifestyle changes and various medicines haven't helped. Surgery aims to provide a cure by tightening the oesophageal sphincter at the top of your stomach. But, as with all surgery, there are associated risks. Talk to your healthcare provider to find out the best treatment options for you.
Apps reviewed by Healthify
You may find it useful to look at some Digestive health apps, Nutrition, exercise and weight management apps, and Quit smoking apps.