If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Melanoma | Mate pukupuku kiri manauri
Key points about melanoma
- Melanoma (mate pukupuku kiri manauri) is a type of skin cancer.
- It often appears as a new spot on normal skin or develops from an existing mole.
- Melanoma is the most dangerous type of skin cancer. If left untreated, it can spread rapidly to other parts of your body and become life-threatening.
- However, if melanoma is recognised and treated early enough, it's almost always curable.
- Aotearoa New Zealand has one of the highest rates of melanoma in the world and has the highest mortality rate.
- If you notice any new spots or darker, growing or changing moles, get them checked straight away.

Melanoma is a type of cancer that begins in your skin's pigment cells, which are known as melanocytes.
Melanocytes produce a brown-coloured pigment called melanin. This gives skin its colour. When melanocyte cells group together in the skin they can form a mole.
Most moles are harmless. However, sometimes the melanocytes in them begin to grow and divide in an uncontrolled way and form a melanoma.
Melanoma is the most serious type of skin cancer and it can spread quickly. It's treatable if it's caught early, but if it spreads to other parts of your body, it can be life-threatening.
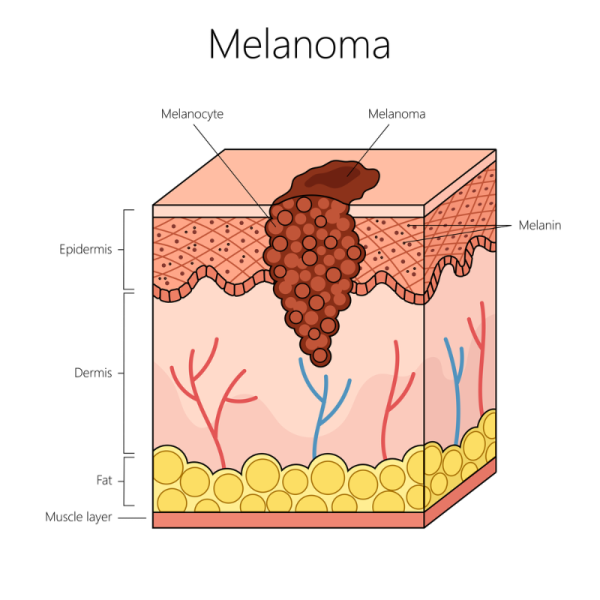
Image: Depositphotos
Most melanomas are caused by overexposure to sunlight, or more specifically UV radiation. Each time your unprotected skin is exposed to UV radiation from the sun or other sources, such as sunbeds, the UV radiation causes changes to the structure of the melanocytes. This causes your skin to become permanently damaged. The damage worsens with more UV radiation.
Some melanomas are inherited (passed down form a parent) but these are much less common.
The main risk for skin cancer is regular unprotected sun exposure
Other factors that may contribute to skin cancer and melanoma, include:
- having a family or personal history of skin cancer
- having fair skin
- having red, blonde or fair hair
- having a skin type that burns easily
- skin damage from sunburn
- use of sunbeds, lamps etc
- having many moles and larger moles
- having a suppressed immune system.
See scan your skin(external link) to find out if you're at risk of skin cancer.
Melanoma occurs most commonly on parts of your body that have been sunburned. However, it can appear in skin anywhere on your body – even on parts that aren’t usually exposed to the sun, such as the soles of your feet or under your toenails.
Types of melanoma include:
- Melanoma in situ – early stage melanoma that hasn’t invaded into deeper tissues. This appears as a smooth, slowly growing or changing patch of discoloured skin.
- Superficial spreading melanoma – the most common type of melanoma. This is a flat discoloured lesion that grows slowly over months to years.
- Nodular melanoma – the second most common type of melanoma. It’s usually a firm, raised, uniformly coloured and often non-pigmented nodule that grows and becomes more raised. It can grow rapidly, over weeks to months.
- Amelanotic melanoma – this type of melanoma doesn’t have any pigmentation. It usually looks red, pink or rash-like.
- Acral and subungual melanoma – these types are both common in people with darker skin, including Māori and Pacific Peoples. Acral melanoma appears on the palm of hands and soles of feet and isn't related to sun exposure. Subungual melanoma occurs under your nails.
- Ocular melanoma – this is a rare melanoma affecting your eye.
- Mucosal melanoma – a rare type that occurs on mucosal surfaces (moist surfaces that line the cavities inside your body) such as in your nose, mouth, gut or genitals.
A melanoma can:
- appear as a new spot or mole
- be an existing spot, freckle or mole that changes colour, size or shape
- sometimes be itchy or bleed
- look different to other spots
- be raised (sticking out) and look shiny
- appear quickly.
See your healthcare provider if you have a skin lesion, such as an unusual looking freckle or mole that is:
- changing – growing in size, changing shape or colour
- sometimes itchy
- not healing – ulcerated or bleeding
- painful or tender to touch.
Some melanomas may not have any pigment (colour). These are called amelanotic melanoma.
If you're worried that you have a melanoma, see your doctor or a qualified skin check provider(external link) for an examination. They will take a thorough history and examine your whole body for possible skin cancers. They should use a dermatoscope, a hand-held device that's used to look more closely at your skin. If they think your mole or skin spot is suspicious, they may arrange to take a small sample of your skin, known as a biopsy, and may arrange a tele-dermatological assessment with a dermatologist (a doctor who specialises in skin conditions).
A biopsy is a simple procedure where a part or all of the skin spot is surgically removed and sent to the lab for testing. This can sometimes be done at your doctor's surgery or you might be referred to a dermatologist or surgeon.
The results will be sent back to your doctor, who will let you know if melanoma or another type of skin cancer was found. If melanoma is found, your doctor will talk to you about any further tests or treatment that's needed.
A tele-dermatological assessment involves taking specific images of the skin spot. These are then securely electronically transferred to a specially trained dermatologist, who can assess them and help diagnose whether the spot is a melanoma or not. This has the advantage of avoiding a biopsy when it's not needed, while making sure all melanomas are excised (cut out) quickly.
Stages of melanoma
- Stage 0 – (melanoma in situ) abnormal cells found in the epidermis (outer layer of your skin).
- Stage 1 – the melanoma is not more than 2 mm thick.
- Stage 2 – the melanoma is more than 2 to 4 mm thick with no spread to your lymph vessels or lymph nodes.
- Stage 3 – any thickness of melanoma that has spread to your lymph vessels or lymph nodes.
- Stage 4 – the melanoma has spread to other parts of your body.
If a melanoma is caught early, it can usually be treated successfully. If it's spread to other parts of your body, it can be harder to treat.
If you have early stage melanoma (stage 0, 1 or 2), surgery is the most common treatment and can cure the cancer. This is usually done by wide local excision (WLE), which means cutting the melanoma out with the aim of removing all of the melanoma cancer cells. A dye may be injected at the time of the WLE to track any drainage to a lymph node.
If you have advanced melanoma that has spread to other parts of your body (stage 3 or 4), you may need a combination of surgery, medicines and radiation therapy.
- Targeted therapy: These medicines block the action of particular molecules that help cancer grow. If the melanoma you have has a BRAF gene change (mutation), targeted therapy options that are funded now include dabrafenib and trametinib.
- Immunotherapy: Medicines such as pembrolizumab (Keytruda) boost your own immune system to attack the melanoma. In some cases other medicines, including infliximab (Remicade) and tocilizumab (Actemra), may be used to treat serious side effects from immunotherapy. Funding for these has recently been extended. .
If your melanoma has spread to your lymph nodes, these may be removed by surgery.
Follow-up
After your melanoma has been treated, you should have regular follow-up appointments so that recurrences (melanoma that comes back after it’s been treated) or new melanomas can be detected. The frequency of follow-up visits will depend on the stage of your initial (primary) melanoma.
You should also check your own skin every month to look for recurrences or further suspicious lesions.
Read more about treatment of skin cancer.
There are things you can so to reduce your risk of getting a melanoma:
- Protect your skin from the sun. Read more about sun safety.
- Don't use sunbeds or sunlamps.
- Get your skin checked by your healthcare provider and do regular self-checks. Learn how to check your skin for skin cancer. See how to check your skin for skin cancer.
Ways to protect your skin
- Avoid outdoor activities when the sun is strongest – between 10 am and 4 pm during September to April in Aotearoa New Zealand.
- Wear sunscreen and lip balm daily that offer SPF 30 or higher sun protection.
- Use sunscreen that offers broad-spectrum (UVA/UVB) protection and is water resistant. Read more about how to choose and use sunscreen.
- Apply the sunscreen and lip balm to dry skin 15 minutes before going outdoors.
- Apply the sunscreen to every part of your body that will not be covered by clothing. Reapply it every 2 hours if you're swimming or sweating.
- Whenever possible, wear a wide-brimmed hat, long sleeves and long pants.
- Wear sunglasses to protect your eyes and the skin around your eyes.
- Avoid sunburn and never use a tanning bed or sun lamp.
Read more about how you can reduce your risk of skin cancer.
Melanoma New Zealand(external link) has a dedicated mobile spot check van, enabling New Zealanders around the country to have free skin cancer spot checks. Find out when it's next in your area(external link).
If found and treated early, most melanomas are curable. The key is to have any skin changes or moles checked straight away.
There are a variety of smart phone apps that are marketed for skin checking and early melanoma detection. They allow you to take photos of your skin, and track and monitor changes to your skin lesions.
Be aware that not all skin checking apps are reliable. Apps that give you a risk assessment of your skin changes by letting you send images to a skin specialist for analysis are far more reliable and a safer option than apps that use automated computerised analysis algorithms to give you an analysis of skin cancer risk.
Read more about skin check apps.
If your melanoma is found early and is surgically removed it’s likely you may never get another melanoma. However, if you’ve had a melanoma, your chance of getting a second primary melanoma is higher than if you’d never had one. This means it’s important to keep checking your skin regularly so that any further melanomas can be picked up early and successfully removed. If you’ve had a melanoma you’re also at higher risk of other types of skin cancer.
The risk of a recurrence (where your melanoma comes back after it’s been treated), is higher if your first (primary) melanoma was:
- thick
- ulcerated (a sore that doesn’t heal, bleeds easily and crusts over)
- a quick growing one (how fast the cancer cells are dividing and growing is known as the mitotic rate, which is measured in the lab when the skin cells are analysed).
Advanced melanoma is a serious condition and a cure is not always possible. The outcome will depend on things such as where the cancer has spread to, how well you respond to treatment and your overall health. Your healthcare provider will be able to help you understand your treatment options.
Melanoma New Zealand(external link) focuses on early detection, prevention, and patient care for people with melanoma. They offer a range of services:
- They have skilled nurse educators who offer free online and telephone consultations to anyone concerned about melanoma and who want advice, support and links to other services.
- They also offer free online counselling and have support group sessions.
The Cancer Society(external link) offers a range of services to help people with cancer, including those with melanoma. There is free cancer information helpline (0800 226 237) available Monday to Friday 8.30 am to 5 pm, or you can email a nurse at [email protected]. They can also provide one-on-one emotional and practical support to people with cancer and their whānau and friends.
Sunsmart(external link) Cancer Society, NZ
Melanoma of the skin(external link) Cancer Society, NZ
All about melanoma(external link) Melanoma New Zealand
Brochures
Finding skin cancer early could save your life – here's how to self-check(external link) Melanoma New Zealand and Cancer Society, NZ. 2021
Check your skin(external link) Sunsmart, NZ, 2019
Early stage melanoma of the skin – Wāhanga tōmua tonapuku ke te kiri(external link) Cancer Society, NZ, 2018 English/te reo Māori(external link)
Advanced melanoma of the skin – Tonapuku maukaha o te kiri(external link) Cancer Society, NZ, 2018 English/te reo Māori(external link)
Advanced melanoma – Tonapuku o te kiri(external link) Cancer Society NZ, 2019
Eye – ocular melanoma(external link) Cancer Society, NZ, 2020
Understanding early melanoma – a guide to early melanoma(external link) Melanoma New Zealand, 2018
Understanding advanced melanoma – a guide to stage III and IV melanoma(external link) Melanoma New Zealand, 2025
Apps and tools
Skin care (dermatology) apps
Skin check apps
Scan your skin(external link)
References
- Melanoma(external link) DermNet, NZ, 2022
- Melanoma(external link) Auckland Region HealthPathways, NZ 2021
- Surviving melanoma(external link) DermNet, NZ, 2013
Clinical guidelines and resources
Reducing the burden of melanoma in NZ Part 1 – prevention and risk assessment(external link) BPAC, NZ, 2020
Reducing the burden of melanoma in NZ Part 2 – early detection of melanoma(external link) BPAC NZ, 2020
Clinical practice guidelines for the diagnosis and management of melanoma(external link) Cancer Council, Australia
Images of melanoma(external link) DermNet, NZ
Melanoma risk calculator(external link) BPAC, NZ
Melanoma(external link) B-QuiCK BPAC, NZ
Quality statements to guide melanoma diagnosis and treatment in New Zealand National(external link) Melanoma Working Group and MelNet, NZ, 2023
- There is a 6-part webinar series(external link) based on the 2nd edition of the Melanoma Quality Statements.
- There is a Goodfellow Unit podcast(external link) based on the latest (3rd) edition of the Melanoma Quality Statements.
See our page skin cancer for healthcare providers
Prevention and early detection strategy
Skin cancer prevention and early detection strategy 2024–2028(external link) Developed by MelNet with support from skin cancer experts and sector stakeholders. The 2024–2028 strategy provides a roadmap to reduce the incidence and impact of skin cancer in New Zealand by outlining 12 key recommendations.
Bringing together healthcare providers, educational organisations, workplaces, sporting and recreational bodies, community and advocacy groups, and local and central government, this unified approach aims to create meaningful change, saving lives and reducing healthcare costs.
Continuing professional development
PHARMAC Seminar series
Videos from the one-day PHARMAC seminar(external link) on dermatoscopy held in Wellington on 4 May 2016, by Prof Bruce Arroll and Prof Amanda Oakley
Dermatoscopic patterns and diagnosis updates (9 videos)(external link) PHARMAC Seminar Series, NZ, 2016
The Skin Cancer College Australasia(external link) also provides education for medical practitioners.
Brochures

Finding skin cancer early could save your life – here's how to self-check
Melanoma New Zealand and Cancer Society, NZ, 2021
Understanding early melanoma
Melanoma New Zealand, 2018

Understanding advanced melanoma – a guide to stage III and IV melanoma
Melanoma New Zealand, 2025
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Melanoma New Zealand
Last reviewed:
Page last updated:





