You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Basal cell carcinoma | Mate pukupuku kiritai
Also known as rodent ulcers
Key points about basal cell carcinoma (mate pukupuku kiritai)
- Basal cell carcinomas (BCCs) are a type of non-melanoma skin cancer.
- They're the most common and the least serious form of skin cancer – as long as they're found and treated.
- BCCs often appear as a pale, pink or pearly smooth lump.
- They're more common among older people, but can develop in younger people.
- Most are caused by long-term exposure to ultraviolet (UV) radiation from sunlight, so they're generally found on parts of your body that get the most sun.
- They tend to be slow growing and very rarely spread to other parts of your body, but can cause significant damage to the surrounding tissues where they grow.

Basal cell carcinomas (BCC) occur when a mutation occurs in the DNA of basal cells in the epidermis of your skin (the outermost layer of your skin). Basal cells produce new skin cells as old ones near the surface die off and are shedded (fall off). Prolonged sun exposure is the main cause of damage leading to BCC. As a result, almost all BCCs occur on parts of your body that get the most sun, such as your face, ears, neck, scalp, shoulders and back.
They occur less often on other parts of your body or legs. Rarely, they can appear on parts of your body that are normally protected from the sun.

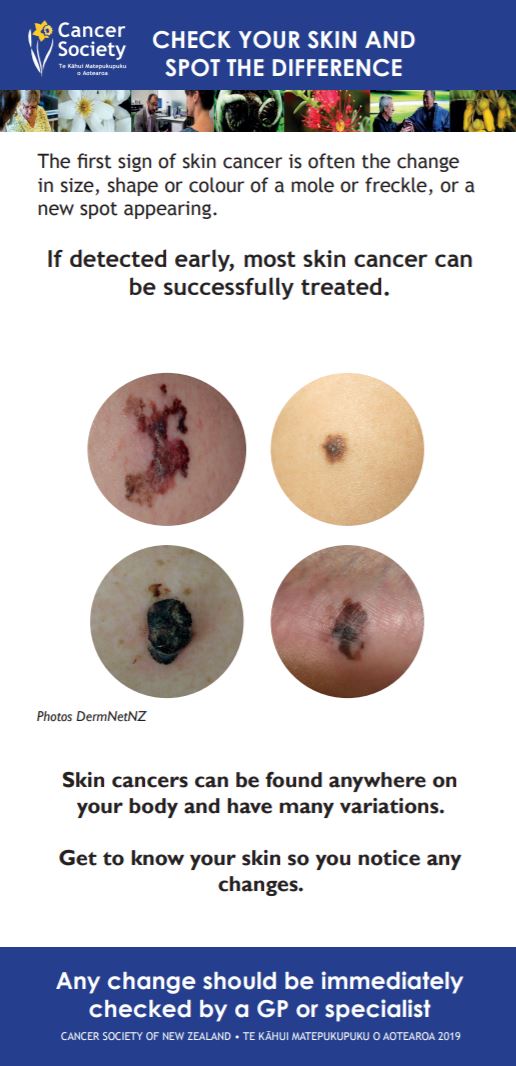
Image source: DermNet NZ(external link)
The main cause of damage leading to BCC is sun exposure. This is usually a combination of:
- long-term, everyday sun exposure, and
- occasional intense exposure, such as severe sunburns.
Sometimes they can result from damage caused by things such as burns, scars, infections, vaccinations or tattoos.
You are at highest risk of developing a BCC if you:
- are older
- have pale skin and burn easily
- have spent a lot of time outdoors for work or leisure
- live in a sunny climate
- use sunbeds or sunbathe
- have previously had a basal cell carcinoma or another type of skin cancer
- have a condition or take medicines that weaken your immune system (immune suppression).
BCCs often appear as a change in your skin, such as a lump or a sore that doesn't heal.
The main features are:
- slow growing – months to years
- a pearly white, skin-coloured or pink bump that is translucent (you can see a bit through the surface)
- waxy, small, raised lesions that may have a dent in the centre
- brown or blue-black areas, in some cases
- a scaly red flat mark on the skin, in some cases
- a tendency to bleed or turn into an ulcer
- scaly, oozing or crusted areas
- varying in size from a few millimetres to several centimetres in diameter.
Apps reviewed by Healthify
You may find it helpful to look at the DermDiag app.
If you notice a change to or growth on your skin, make an appointment to see your healthcare provider straight away. They will assess the size, location and appearance of the growth. They will also ask you how long you have had it, whether it bleeds or itches, etc.
If your healthcare provider thinks the growth looks suspicious and may be cancer, they may take a small sample of tissue (a biopsy). The tissue sample will be sent to a laboratory and examined under a microscope. Your healthcare provider will let you know whether the sample showed any cancer cells, and will recommend appropriate treatment if necessary.
Treatment of a basal cell carcinoma depends on its type, size and location and other factors, such as your preference.
Options include:
- Surgical removal of the cancer (this is the most common treatment method).
- Freezing it with liquid nitrogen (cryotherapy).
- Radiotherapy.
- Topical therapies (creams) such as Imiquimod or Fluorouracil cream.
- Photodynamic therapy (a specialist treatment using light to activate creams).
If you have a BCC, your healthcare provider will discuss treatment options with you. Treatment will almost always cure a BCC, as long as it's found at an early stage. You may need to plan a future appointment to check for recurrences, new skin cancers or precancerous changes.
Read more about skin cancer treatment.
Most basal cell carcinomas can be treated and cured. However, these types of cancers can recur and new skin cancers may appear.
Do the following to reduce the risk of new cancers occurring:
- Keep all follow-up appointments with your healthcare provider or skin specialist.
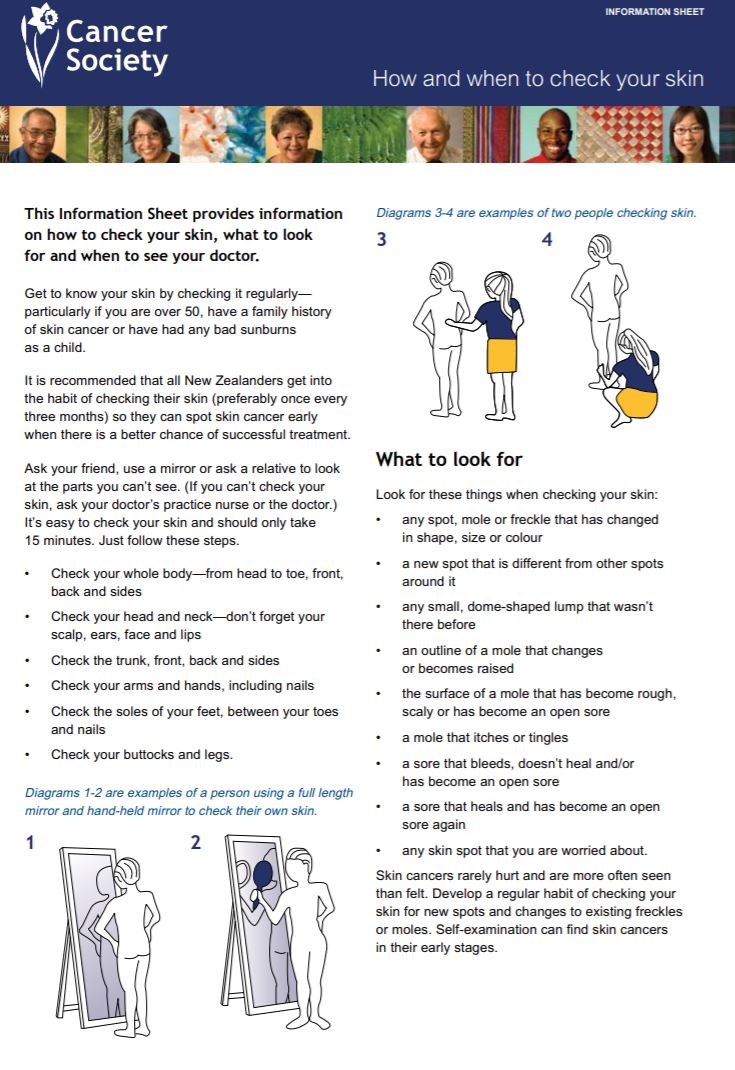
- Regularly check all your skin (from head to toe). If you see anything that is growing, bleeding or in any way changing, go and see your healthcare provider straight away. Read more about how to do skin cancer checks.
- Protect your skin from the sun and avoid indoor tanning. This is essential to prevent further damage, which will increase the risk of getting another skin cancer.
Ways to protect your skin
- Avoid outdoor activities when the sun is strongest – between 10am and 4pm from September to April in Aotearoa New Zealand.
- Wear sunscreen and lip balm daily that offer SPF 30 or higher sun protection.
- Use sunscreen that offers broad-spectrum (UVA/UVB) protection and is water resistant.
- Put sunscreen and lip balm on dry skin 15 minutes before going outdoors.
- Apply the sunscreen to every part of your body that won't be covered by clothing. Reapply it every 2 hours if you're swimming or sweating.
- Whenever possible, wear a wide-brimmed hat, long sleeves and long pants.
- Wear sunglasses to protect the skin around your eyes.
- Avoid getting a tan and never use a tanning bed or sun lamp.
See more information on sun safety.
Apps reviewed by Healthify
You may find it useful to look at some Sun safety apps.
Basal cell carcinoma(external link) DermNet NZ
Basal cell carcinoma(external link) Skintel, NZ, 2022
Brochures
Check your skin and spot the difference(external link) Cancer Society, NZ, 2019 English and te reo Māori
Basal cell carcinoma patient information sheet(external link) British Association of Dermatologists
Apps
References
- Telfer NR, Colver GB, Morton CA. Guidelines for the management of basal cell carcinoma(external link) Br J Dermatol. 2008;159:35–48
- Basal cell carcinoma(external link) DermNet, NZ(external link)
- Skin lesion excision(external link) Auckland Regional HealthPathways, NZ, updated 2023
Brochures
Cancer Society, NZ, 2019
Cancer Society, NZ, 2010
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Lottie Wilson, General Practitioner, Queenstown
Last reviewed:





