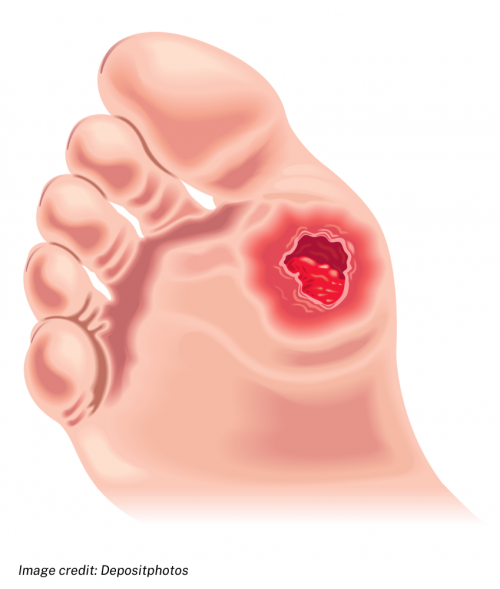
A foot ulcer is an open sore or wound on your foot that is slow to heal because of your diabetes, and sometimes there are circulation problems too.
If it gets infected it can be very serious.

We're aware of a problem when trying to use Zero Data to link to Healthify. Zero Data is managed by Health NZ and we are working with them to get this fixed.

A foot ulcer is an open sore or wound on your foot that is slow to heal because of your diabetes, and sometimes there are circulation problems too.
If it gets infected it can be very serious.
If you have diabetes you have a greater chance of developing foot ulcers because you’re more likely than other people to not notice if you damage the skin on your feet. This is because diabetes can cause nerve damage, so you don't notice if your foot is injured or sore. Diabetes also causes sores to heal slowly and causes blood vessel damage so your skin can't heal easily.
Foot ulcers are open sores or wounds that occur most often on the ball of your foot or on the bottom of your big toe. They may also develop on the side of your foot, usually because of poorly fitting shoes. The ulcers are usually painless. Not all diabetes-related foot ulcers become infected but if you have diabetes you are at high risk of developing infection of the ulcer and the surrounding skin (cellulitis). Infected diabetes-related ulcers are a serious problem and need urgent attention.
Depending on the severity of the wound and the presence of infection, diabetes-related foot ulcers can be classified in 4 ways:
If you have diabetes and notice a sore or blister on your foot, contact your healthcare provider immediately. If ulcers aren't treated it can result in infection, which can cause loss of a limb. This can be avoided if you take care of your feet and act quickly if you have a problem.
Treatment of the foot ulcer depends on the severity of the wound.
Severity |
Treatment |
|
All |
|
|
Not infected |
|
|
Mild infection |
|
|
Moderate infection |
|
|
Severe infection |
|
In addition to managing the wound, attention to other lifestyle factors can also contribute to improved wound healing.
You may find it useful to look at some Diabetes apps.
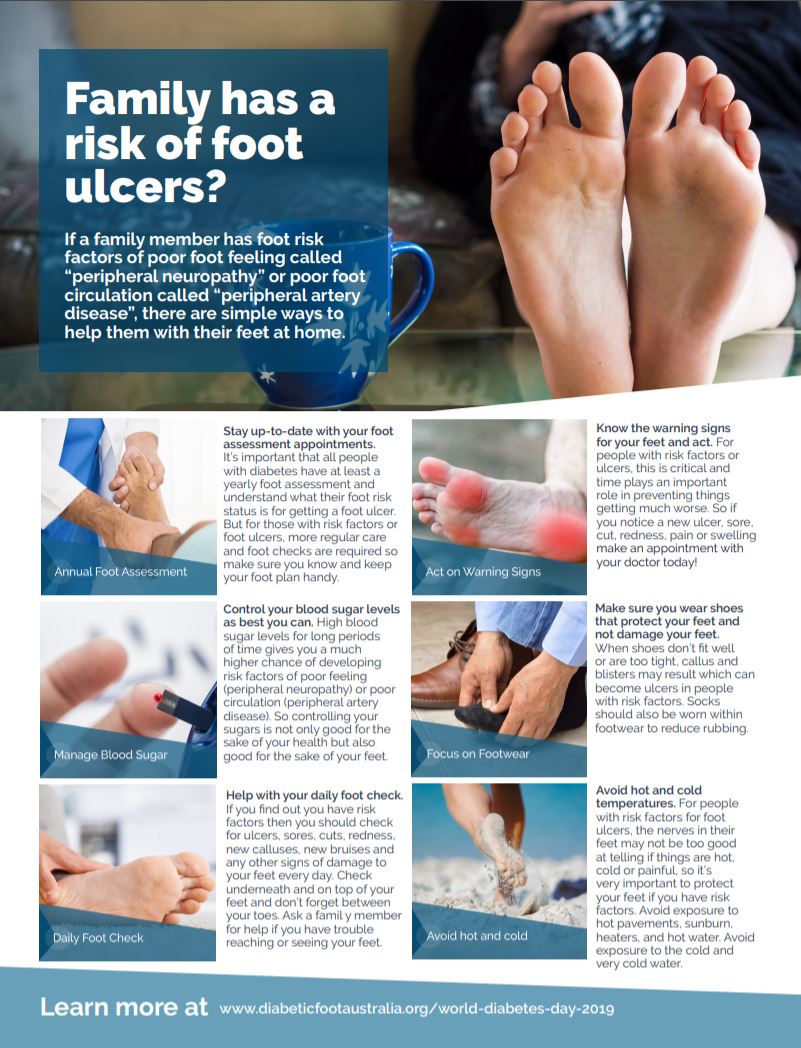
You can lower your risk of developing diabetes-related foot problems by:
Learn more about diabetes and foot care.
When you have diabetes, it's important to take extra care of your feet to prevent ulcers and other complications.
If the foot ulcer doesn't heal, becomes worse or badly infected, or if the infection spreads to nearby bones or joints, this can lead to gangrene. The only solution then may be to surgically remove (amputate) the affected part.
There are many groups and people keen to share their knowledge and tips for living well with diabetes. Diabetes New Zealand(external link) has branches around the country with a wide range of services, resources, groups and shops.
The following links provide further information on diabetic foot ulcer. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Diabetic foot ulcers(external link) DermNet NZ
Diabetes, foot care and foot ulcers(external link) Patient Info, UK
The right steps to healthy feet(external link) Diabetes New Zealand
Feet(external link) Diabetes New Zealand
Diabetes and foot problems(external link) Diabetes UK
Type 2 diabetes – health problems(external link) NHS, UK
Diabetes feet care checklist(external link) Diabetes Feet Australia
Know your risk diabetes(external link) Diabetes New Zealand
Diabetes and how to care for your feet(external link) Diabetes New Zealand
Family has a risk of foot ulcers?(external link) Diabetic Foot Australia
Best Practice diabetes toolbox(external link) BPAC, NZ, 2021
Diabetes (the high risk foot)(external link) NZ Society for Study of Diabetes (NZSSD), Podiatry Special Interest Group (PodSIG), NZ, 2017
Primary care/district nursing diabetic foot assessment form(external link) Diabetic Foot Ulcer Group, NZ, 2011
Secondary care diabetic foot ulcer assessment Form(external link) Diabetic Foot Ulcer Group, NZ, 2011
Diabetes feet health passport(external link) Diabetes Feet Australia
IWGDF guideline on the prevention of foot ulcers in persons with diabetes(external link) International Working Group on the Diabetic Foot Guidelines, 2019
IWGDF guideline on offloading foot ulcers in persons with diabetes(external link) International Working Group on the Diabetic Foot Guidelines, 2019
See our page Diabetes for healthcare providers
Diabetic foot disease(external link) Goodfellow eLearning, NZ, 2019
Diabetic Foot Australia, 2019
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Michele Garrett, Professional Leader Podiatry | Te Toka Tumai, Waitematā & Metro Auckland Foot Protection Services
Last reviewed: