Dementia | Mate wareware
Key points about dementia
- Dementia (mate wareware) is a group of symptoms which happen when brain function declines.
- It includes problems with memory, thinking, behaviour and the ability to perform daily tasks.
- Dementia is more common in people over 65 years of age, but it's not a normal part of ageing.
- If you're becoming more and more forgetful, especially if you're over 65, talk to your healthcare provider about the early signs of dementia.
- Getting a diagnosis can help you to plan for the future and get the right support and advice.

Dementia is a group of related symptoms caused by an ongoing decline of your brain. It’s different from occasionally losing your keys or forgetting a name.
It may include problems with:
- memory
- thinking
- language and understanding
- mood
- behaviour.
As these symptoms get worse, they can make it difficult for you to carry out your normal daily activities.
Dementia happens because of damage to brain cells. Which symptoms you get depends on which areas of your brain have been damaged. It's progressive, meaning the symptoms gradually get worse over time.
Dementia is more common in people over 65 years of age, but it's not a normal part of ageing. More than 70,000 people in Aotearoa New Zealand have dementia. It’s getting more common as we live longer.
There are different types of dementia. The most common is Alzheimer's disease, which affects about 60% of people with dementia. Other types of dementia are vascular dementia, Lewy body dementia, frontotemporal dementia and alcohol related dementia. You can also have ‘mixed’ dementia – a mixture of Alzheimer's disease and vascular dementia.
Early onset dementia (or young onset dementia) describes dementia that occurs in people under 65 years of age. About 5% of people who develop dementia have early onset dementia.
Video: Dementia educational video
Dementia is due to damage and eventual death of cells in the brain. This can be caused by head injury, damage to your brain's blood vessels from diabetes, smoking or a stroke (vascular dementia), or damage from toxins such as alcohol. In Alzheimer’s disease the exact cause of the damage is not known. Once cells die, they're not replaced.
Most dementia is not inherited. However, in rarer types of dementia such as frontotemporal dementia, there may be a strong genetic link. These make up only a tiny proportion of overall cases of dementia.
The older you are, the greater your chance of getting dementia. Most people are over 65 years of age when they're diagnosed.
There are some groups of people who are known to have a higher risk of developing dementia. These include people with:
- Māori and Pacific ancestry
- risk factors for cardiovascular disease (eg, angina, heart attack, stroke and peripheral arterial disease)
- Down syndrome
- Parkinson's disease
- a history of drinking too much alcohol
- a family history of dementia
- a history of a head injury
- mental health conditions, such as schizophrenia or severe depression
- low physical activity levels.
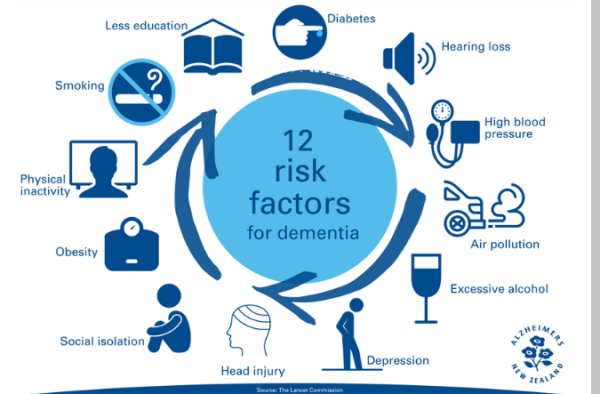
Image credit: Alzheimers NZ

Image credit: Alzheimers NZ
Recent research has added 2 more risk factors for dementia to the 12 in the image above. The 2 new ones are high LDL cholesterol and vision loss. It's suggested that almost half of dementia worldwide could be prevented or delayed if these risk factors were addressed.
Dementia symptoms affect 3 main areas:
- mental ability
- mood, personality and behaviour
- day-to-day activities.
Symptoms can include:
- forgetting things that happened recently (things that happened a long time ago are usually remembered better)
- repeating questions
- not remembering appointments
- often forgetting people’s names, or the names of things around the house
- not being able to plan the steps to do everyday tasks, eg, making a meal or getting dressed
- disorientation – not knowing what time of day it is, or what is appropriate for that time of day
- not being able to start or carry on a conversation, or get started on something you once enjoyed
- moods changing very quickly for no apparent reason
- problems with abstract thinking – trouble understanding ideas or concepts.
If you, or someone you care for, are becoming increasingly forgetful, it may be a good idea to talk to your healthcare provider about the early signs of dementia. It’s a good idea to take someone who knows you well to your appointment. Your healthcare provider will talk with you about what you've been experiencing, and what your whānau and friends have noticed. They will guide you through a memory test.
To check for other causes of your symptoms you will need to have a blood test. A small number of people will need to have a CT scan. It may take a few appointments to get a good understanding of what is going on for you. Usually your own healthcare provider will be able to diagnose dementia, but if it's not clear they may refer you to a health professional who specialises in dementia for further assessment.
Although there's no cure for dementia, there are many things you can do yourself and with your whānau and friends to continue to enjoy your life. These include:
- getting support – contacting a dementia support organization as soon as you know you or your family member has dementia is one of the most helpful things you can do.
- making lifestyle changes
- doing mind and memory-based activities.
- cognitive stimulation therapy.
Lifestyle changes
It isn't possible to prevent dementia gradually worsening, but there are things you can do to keep your brain cells as healthy as you can:
- Get some exercise most days
- Avoid smoking, alcohol and other substance use. If that’s not possible, cut down.
- Eat a healthy diet
- Get enough sleep.
Mind and memory-based activities
These could include:
- keeping up your social activities – they’re good brain exercise, and loneliness makes brain function worse. If you have hearing loss, this might mean getting a hearing aid.
- cognitive rehabilitation, where a health professional helps you achieve a goal, eg, learning to use a mobile phone
- life story work, where you use a scrapbook, photo album or electronic app to remember and record details of your life
- music and creative arts therapies to keep your brain active and help you express your emotions
- sensory stimulation such as aromatherapy, massage or bright light stimulation – discuss these with your healthcare provider beforehand
- doing brain exercises such as puzzles, and practicing memory strategies.
Cognitive stimulation therapy
Cognitive stimulation therapy (CST) is a structured group treatment developed for people with mild to moderate dementia. It consists of 14 sessions with a range of activities and discussions aimed at improving your mental and social functioning. The sessions actively engage people with dementia, providing a good learning environment and the social benefits of being part of a group. CST has been found to be helpful for older people with a clinical diagnosis of mild to moderate dementia.
Arrange a care planning meeting
Plan ahead so that you have more say in your future. Arrange a meeting (or get someone else to do it) with all the people involved in your care. This may include your carer, whānau members, or your doctor or nurse.
Agree on a care plan to support you to stay as well as possible for as long as possible. This might include:
- having a driving assessment
- arranging enduring power of attorney
- writing or updating your will
- developing an advance care plan
- accessing services to help you stay independent for as long as possible
- learning about your condition.
Read more about these below.
Having a driving assessment
Driving requires quick reflexes and decision making. Having a driving assessment will help you work out whether it's safe for you to continue driving for now, and if not, how you will manage without driving. Read more about dementia and driving and ways to manage without a car.
Arranging enduring power of attorney
Having an Enduring Power of Attorney (EPA) means you can have peace of mind that you have decided, ahead of time, who you trust to make decisions for you if you can’t decide for yourself. Read more about enduring power of attorney.
The Public Trust(external link) offers free 30 minute consultations for people with dementia, their families and caregivers. To book an appointment phone 0800 371 471.
Writing or updating your will
A will sets out your wishes in terms of who to leave your possessions and money to and states who you would like to carry out your wishes. It can include special instructions for a funeral. If you don’t have a will, it could also put your family into legal and financial difficulties. Learn more about making a will.(external link)
Developing an advance care plan
An advance care plan is a way to record your wishes for your current and future medical care. It's an ongoing process of talking with those closest to you and getting information to help you make decisions about your care. It can include end of life planning. Read more about advance care planning.
Learning about your condition
Learning about dementia can help you plan for the future as well as stay independent for as long as possible. You will find resources and other links under More information below. It’s important for your family to understand what’s happening, so they can help you and also keep themselves well. There's information about this on our dementia for caregivers page.
Apps reviewed by Healthify
You may find it useful to look at some dementia apps, exercise apps for older adults, and carer support apps.
Treating heart risk factors
Management of heart risk factors may benefit all types of dementia. Generally, what's good for your heart is good for your brain. Read about heart risk assessment.
Medicines
There are medicines that can help some people with the symptoms of forgetfulness and improve their ability to think more clearly in the earlier stages. Medicines don’t cure dementia and they may only work for some people. The aims of treatment are to promote independence, maintain function and treat symptoms. These medicines fall into 2 categories:
- cholinesterase inhibitors (eg, donepezil, rivastigmine and galantamine)
- memantine.
These work by enhancing the levels of a chemical in the brain (called acetylcholine), that's involved in memory and judgment. Read more about medicines for dementia.
Your healthcare provider will also review any other medicines you are taking to check that they're not contributing to any symptoms similar to those of dementia.
Find your local Alzheimer's branch(external link) NZ
Dementia NZ(external link)
For other support services for people with dementia, their carers and for healthcare providers see the dementia support page.
You may have dementia for years before it's recognized, and every person with dementia is different. Some people live for decades with dementia, but the average lifespan after diagnosis is 5 to 12 years depending on the type.
Usually in the first few years you’re able to live at home with support and enjoy most of the things you used to. It’s important that your whānau are cared for as well. Read more about dementia for carers and carers need care too.
As time goes by more care is needed. Your healthcare provider can co-ordinate practical supports for you – such as occupational therapy – and financial supports for your caregiver if you’re eligible.
In the later stages of dementia you may have problems with speech, eating, mobility and continence. This may mean you need residential care. Dementia does shorten your life span, but often it's another health problem that's the cause of death, eg a chest infection.
Video: Living well with dementia – Helen's story
Video: Living well with dementia – Peter and Fergus' story
Video: Memories and forgetfulness – Colin's story
(Alzheimers NZ, 2016)
Video: Yep, my dad has dementia – Victoria's story
(Alzheimers New Zealand, 2016)
Video: Unexpected positives of dementia | 'My story hasn't ended...only the ending has changed'
(Alzheimer's Australia, 2014)
Alzheimer's disease
Dementia – for carers
Information for carers on managing disruptive behaviour
Driving and dementia
Dementia – preventing social isolation
Reducing your risk of dementia
Ageing – what is normal and when to seek medical advice
Advance care planning
Enduring power of attorney
Dementia topics | Mate wareware
Understanding mate wareware from a Māori perspective(external link) Mate wareware, NZ
Information and support(external link) Alzheimer's NZ
Dementia and the arts – sharing practice, developing understanding and enhancing lives(external link) Future Learn Online Course (paid) 2 hours a week for 4 weeks
Apps
Dementia apps
Exercise apps for older adults
Carer support apps
Resources
Dementia NZ(external link) A variety of information sheets
Promoting and managing continence for people living with dementia mate wareware(external link) University of Auckland, NZ
Living with dementia(external link) Alzheimers New Zealand, 2023
Eat to cheat dementia – what you eat helps you avoid it or live well with it(external link) Ngaire Hobbins
Montessori for dementia, disability and ageing(external link) AMI
Eating well with dementia(external link) Healthinfo, NZ
Harris List(external link) Resources and information on dementia for New Zealanders
Alzheimer's New Zealand(external link) A variety of factsheets (also available in te reo Māori)
Dementia and driving(external link) NZ Transport Agency
Dementia in multiple languages(external link) Health Translation Australia
References
- Memory loss and dementia(external link) Patient Info, UK, 2021
- Can dementia be prevented?(external link) NHS, UK, 2023
- Cognitive stimulation therapy – a New Zealand pilot(external link) Te Pou, NZ, 2014
- The dementia guide(external link) Alzheimer’s Society, UK, 2017
- Dudley M, Menzies O, Elder H, et al. Mate wareware – understanding ‘dementia’ from a Māori perspective(external link) NZ Med J. 2019;132(1503):66-74
- Is dementia hereditary?(external link) Alzheimer's Society, UK
- Recognising and managing early dementia(external link) BPAC, NZ, 2020
Brochures
Alzheimers NZ, 2019

Promoting and managing continence for people with dementia mate wareware
University of Auckland, NZ, 2024
Alzheimers NZ, 2021
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





