You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Cough in children
Key points about cough in children
- Coughing is common in tamariki, especially in preschoolers. Causes include colds, asthma and chest infections.
- Being around smoking and vaping often causes tamariki to cough even when they're well.
- Many tamariki will keep coughing for about 2 to 3 weeks after a cold.
- A cough that lasts more than 4 weeks may be a sign of more serious disease. If your child has a cough that lasts more than 4 weeks, see your healthcare provider.
- If your child has a cough and a fever, or trouble breathing, see a healthcare provider.
- The content on this page comes from KidsHealth(external link).

A cough is a reflex action that tries to clear your airways of mucous (phlegm) and irritants such as dust or smoke. The cough reflex protects your airways and lungs.
Coughing is common in tamariki, especially in preschoolers. Causes include colds, asthma and chest infections.
Being around smoking and vaping often causes tamariki to cough even when they're well.
Coughing is common in tamariki, especially in preschoolers. Tamariki can cough for about 2 to 3 weeks following a cold.
A cough is usually wet or dry.
- Wet cough: A wet cough sounds 'chesty'. You may hear or feel a ‘rattle’ when your child coughs.
- Dry cough: A dry cough can sound irritated, harsh or barking. It’s less likely to produce mucus (phlegm).
Video: Cough-free – the way to be
A chronic persistent wet cough is a serious warning sign and shouldn't be ignored. A long-lasting wet cough can lead to the development of lung diseases such as bronchiectasis. See a video narrated by former Warriors rugby league player Wairangi Koopu. It focuses on knowing the signs of infection that can lead to bronchiectasis. It advises viewers to act on these signs.
(Ministry of Health | Manatū Hauora, NZ, 2016)
Colds (upper respiratory tract infections)
Young tamariki can have several colds each year. Tamariki can keep coughing for 2 to 3 weeks after a cold.
Asthma
An asthma-related cough is usually dry and happens at night, with activity, or in the early morning. Tamariki with an asthma-related cough usually have other symptoms such as wheeze. They may also have eczema or hay fever, or a history of asthma and allergy in the family.
Being around smoking and vaping
Being around smoking and vaping can cause tamariki to cough even when they are well. Make sure your child's environment is smoke-free and vape-free.
If you want to give up smoking or vaping, contact Quitline free on 0800 778 778 or talk with your healthcare provider.
Chest infections
If your child has a wet, chesty, rattly cough and a fever, it's likely to be a chest infection.
Whooping cough
Whooping cough causes long episodes of continuous coughing. 'Whoop' is the sound some tamariki make after they cough and catch their breath.
Whooping cough can cause very serious illness in pēpi and young tamariki. Older tamariki usually get a less severe disease but the cough can be very distressing.
The best protection against whooping cough is vaccination. Whooping cough vaccination is free during pregnancy. It helps protect pēpi in their first weeks of life. Vaccinating pēpi when they turn 6 weeks old helps keep them protected.
Croup
Croup may cause a harsh or barking cough.
Call Healthline on 0800 611 116 or see a healthcare provider if your child has a cough and:
- is having trouble breathing
- is breathing fast
- has a temperature higher than 38°C
- is having trouble speaking
- is wheezing
- you think they could be having an allergic reaction
- you’re worried.
If your child has had a daily cough for longer than 4 weeks, take them to a healthcare provider. A daily cough for more than 4 weeks is not normal and may be a sign of more serious disease.
If your child has a wet cough lasting more than 4 weeks, they may have a more serious disease, such as bronchiectasis. It's very important to recognise this early. Take your child to a healthcare provider.
See a healthcare provider urgently if your child has a cough and:
- is under 3 months of age
- is struggling to breathe
- can’t finish a whole sentence
- is struggling to feed
- you think they’ve choked on something
- you're worried.
Call 111 within Aotearoa New Zealand (use the appropriate emergency number in other countries) and ask for urgent medical help if your child:
- is blue around the mouth
- is unable to breathe
- is hard to wake
- is choking and can’t breathe
- is floppy
- you're worried.
Video: Cough in children (animation in English)
(NZKidsHealth, NZ, 2024)
This video is also available in te reo Māori(external link), Samoan(external link) and Tongan(external link).
Most tamariki with a cough don't need medical treatment. The cough usually gets better within 2 to 3 weeks.

Image credit: Canva
Self-care can help to relieve symptoms and make your child more comfortable
- Avoid cough medicine. Cough medicines are not useful for treating cough. Avoid giving cough medicine to your child unless your healthcare provider recommends it. Read more about cough and cold medicines for children.
- Antibiotics don't help coughing caused by a viral infection. Your health professional may prescribe antibiotics if your child's cough comes from a bacterial infection in the throat or chest.
- Honey may be helpful for a cough caused by a cold. But, wait until your baby is at least 12 months old before giving them honey. It can make young pēpi (babies) sick.
- You can give paracetamol if your child is in discomfort or miserable with a fever. You must follow the dosage instructions on the bottle or packet. It's dangerous to give more than the recommended dose. If you're not sure how much to give, use our paracetamol dose calculator.
There are some things you can do to reduce your child's chances of becoming unwell with a cough.
- Breastfeeding pēpi protects them from illness by boosting their immune system. Breastfeeding beyond 4 months of age offers the best protection.
- Keep your child’s environment smoke-free and vape-free. If you want to give up smoking or vaping, contact Quitline or talk with your healthcare provider or whānau.
- Keeping the house warm, dry and well-insulated also lowers your child’s risk of being unwell with a cough. Read more about keeping your home warm and dry.
- Make sure your child is up to date with all their vaccinations. Vaccination can help prevent many coughing illnesses including:
- Try to keep young pēpi away from people who have coughs and colds.
-
Use hand sanitiser or encourage frequent hand washing with soap and water. This helps reduce the spread of infections.
Brochures
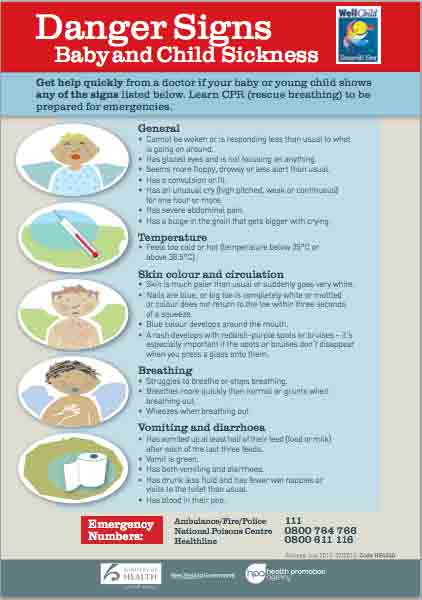
Danger signs – baby and child sickness(external link) HealthEd, NZ, 2013 English(external link), te reo Māori(external link)
Does your child cough?(external link) Starship and Asthma Foundation, NZ, 2012
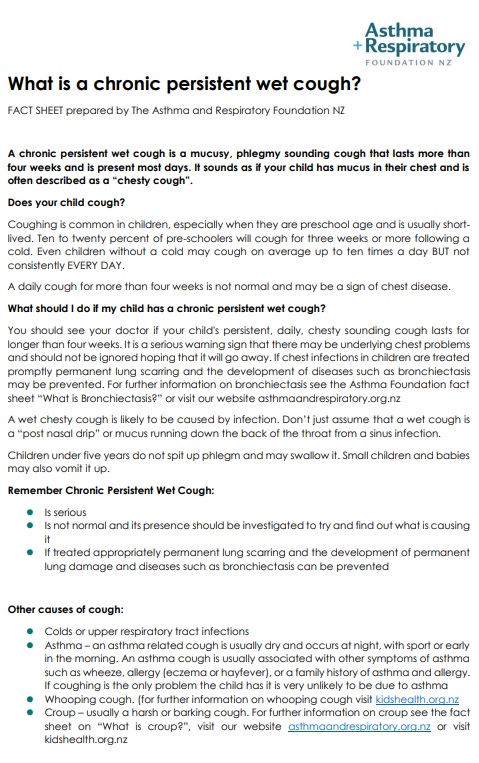
What is a chronic persistent wet cough?(external link) Asthma Respiratory Foundation NZ, 2010
Virus action plan (child)(external link) He Ako Hiringa, NZ, 2023 te reo Māori(external link), Samoan(external link), Tongan(external link), Arabic [PDF, 214 KB], Hindi(external link), Chinese (simplified)(external link)
Clinical resources
Cough(external link) Starship Clinical Guidelines, NZ, 2024
Cough in children guide(external link) BPAC, NZ, 2010
Cough medicines – do they make a difference?(external link) BPAC, NZ, 2023
Clinical pointers – managing recurrent or persistent cough in children under 5(external link) BMJ Learning, The Royal New Zealand College of General Practitioners Modules (requires registration)
Effect of honey, dextromethorphan, and no treatment on nocturnal cough(external link) JAMA Pediatrics
Cough in children – when does it matter?(external link) Paediatric Respiratory Reviews
Chronic cough hypersensitivity syndrome(external link) BioMed Central
Brochures

Virus action plan (child) He Ako Hiringa, NZ, 2023 te reo Māori, Samoan, Tongan, Arabic, Hindi, Chinese (simplified)
Asthma Respiratory Foundation NZ, 2010
Credits: Content shared between HealthInfo Canterbury, KidsHealth and Healthify He Puna Waiora as part of a National Health Content Hub Collaborative.
Last reviewed: