You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Bronchiectasis – children | Pūkahukahu hauā
Key points about bronchiectasis in children
- Bronchiectasis (Bx) is a chest disease – the airways in the lungs have become damaged and scarred.
- Mucus gets trapped in pockets in the airway – this causes infections.
- The main symptoms of Bx are a wet sounding cough that lasts for weeks or happens often, and repeated chest infections.
- Once your child has Bx, they usually have it for life.
- Early recognition and treatment can improve the scarring.
- Good care can help your child to stay well with Bx.
- The content on this page comes from KidsHealth(external link).

You can't catch Bx or give Bx to anyone. Bx is different from asthma but some children with Bx have asthma as well.
Bronchiectasis (Bx) is a chest disease – the airways in the lungs have become damaged and scarred.
The airways (or breathing tubes) become widened and mucus can be trapped in pockets within the airway. Having extra mucus in the airways means bacteria and viruses can grow quickly and cause infections.
These infections cause damage and more scarring to the airways and lungs. Once this has happened, the scarring is usually lifelong. But, with good treatment, there can be some improvement and further damage prevented. Good treatment is especially important in young children because their lungs are still growing.
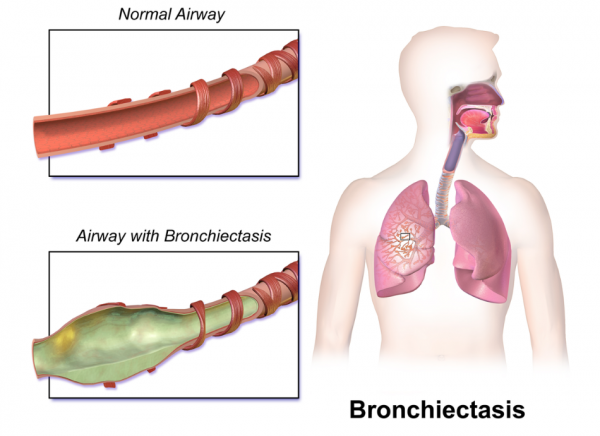
Image credit: BruceBlaus, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Video: Cough-free – the way to be
The following video features former Warriors rugby league player Wairangi Koopu. It focuses on recognising the signs of infection that can lead to bronchiectasis, and acting on them. This video may take a few moments to load.
Common causes
Most children get Bx after having a very bad chest infection or repeated chest infections. Bx usually develops after a child has had:
- severe bronchiolitis or pneumonia needing a hospital stay
- chest infections which need repeated antibiotic treatment at home
- a wet sounding cough lasting for weeks or happening often.
Less common causes
Problems with fighting off infection: Some children can't fight infection very well because they're born with a problem in their infection-fighting (immune) system.
Medicines: Some medicines (eg, oral steroids) cause difficulty in fighting off infection.
Objects stuck in the airway: If a child breathes in a nut or a piece of a toy and this gets stuck in the airway, it can cause a blockage that can lead to scarring.
Food or liquid going into the lungs (aspiration): Children who sometimes cough or choke when feeding have problems controlling their swallow. Food can end up in their lungs. This can also happen if food refluxes from the stomach and ends up going into the lungs. Over time this can cause Bx.
Primary ciliary dyskinesia: In this condition, the tiny mucus-clearing hairs (cilia) in the lungs are not working properly.
How long does bronchiectasis last?
Once a person has Bx, they usually have it for life. Good treatment stops it getting worse and in very young children, can reverse some of the disease.
Who gets bronchiectasis in Aotearoa New Zealand?
- 1 in 3,000 children gets Bx.
- There is 1 new case of Bx in a New Zealand child every week.
Children with Bx feel well most of the time.
Wet-sounding cough
A wet-sounding cough is the main symptom. This usually lasts for weeks. Extra mucus (phlegm or sputum) in the airways causes the cough and your child may spit or cough up some of this mucus.
This cough can get worse during infections, first thing in the morning and during exercise. Remember though that exercise and playing sport is helpful for keeping well.
When children with Bx become unwell, they cough more and the mucus can change colour from clear to yellow or dark green. The mucus can sometimes be smelly. They may lose their appetite and feel tired.
When to see a doctor
If your child has Bx, you should take them to see your healthcare provider when they:
- have a bad cold with a runny green nose
- are coughing more than normal
- have a cough that's wetter than usual
- have more mucus that's darker, thicker or smelly
- are breathing faster than normal
- have a fever
- have pain in their chest
- are tired and not eating or drinking as well as normal
- are unable to take part in sport and exercise.
When to see a doctor urgently
Your child is very sick and needs to see a doctor urgently if they:
- get suddenly more unwell
- cough up blood.
When to dial 111
Dial 111 within New Zealand (use the appropriate emergency number in other countries) for urgent medical help if your child:
- has difficulty talking because they're so short of breath
- has blue lips or tongue
- is coughing up a large amount of blood.
- Chest X-ray: A chest X-ray is usually the first investigation but does not always show Bx damage very well. Your child will probably also need a chest CT scan.
- CT scan: Chest CT scans show Bx damage well.
- Sputum culture: Your healthcare provider will collect some mucus from your child. Many children will be able to cough some mucus into a jar. Sometimes a physiotherapist might need to help your child collect a mucus sample. The mucus is tested for bacteria or viruses. If your child's mucus contains bacteria, your healthcare provider will give them the right antibiotic to treat the infection.
- Blood tests: Your child will have some blood tests to show that they're able to fight off infection.
- Lung function test: Your child will breathe into a machine to measure how well their lungs are working. It usually takes about 15 minutes.
- Bronchoscopy: A doctor can use a special telescope (bronchoscope) to look into the lungs. This lets them see the condition of the airways and take a sample of mucus. This test is done under a general anaesthetic read more about anaesthetics.
- Other tests: Sometimes your child may need other tests such as a sweat test(external link) (to look for cystic fibrosis).
The image shows a lung function test.

Image credit: DataBase Center for Life Science (DBCLS), CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons
Chest physiotherapy
Your child will need chest physiotherapy once or twice a day. There are different ways to do chest physiotherapy – either with breathing and percussion or by using a physiotherapy breathing device (PEP, acapella, bubble). This is to clear the extra mucus from your child's lungs to keep your child well. The physiotherapist will show you the best method to use with your child. The type of chest physiotherapy changes with age.
Exercise and sport
Exercise will help your child – it doesn't matter if they cough. Exercise or playing sport 3–4 times a week is helpful to clear the mucus and to develop your child's lungs. Any type of exercise is good, especially if it makes your child take deep breaths. It doesn't matter if your child coughs during exercise.
Antibiotics
Your child will need antibiotics if they start to get sick or if they are coughing more. Children with Bx need a longer course of antibiotics (10–14 days). Most often, you can give your child antibiotics at home. Sometimes, if your child is very unwell, they may need antibiotics in hospital.
Asthma treatment
Some children with Bx may benefit from inhalers because they also have asthma.
Bx action plan
Children and young people with Bx can have an action plan. You and your healthcare provider or another member of your child's health team can discuss this so that it's right for your child. It lists your child's daily treatment and steps to take if your child becomes unwell.
As an example. here's a bronchiectasis action plan(external link) designed by the Bronchiectasis Foundation.
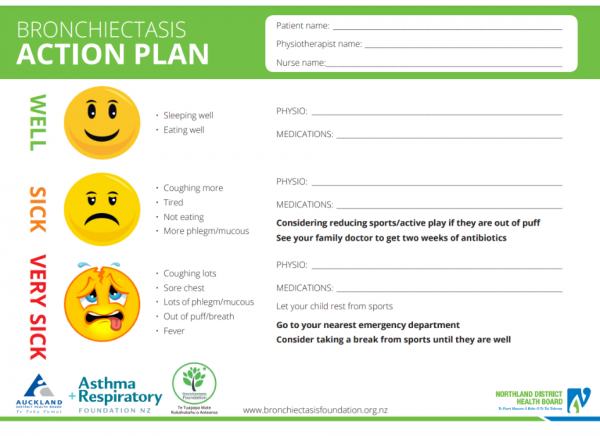
Image credit: Bronchiectasis Foundation, NZ
Things you can do include providing your child with:
- regular physiotherapy to keep their lungs clear of mucus
- regular exercise and sport
- a healthy balanced diet
- a smoke free environment – keep them away from any tobacco smoke, especially in a house or car
- a flu vaccine every year
- regular hospital clinic and healthcare provider reviews.
Apps reviewed by Healthify
You may find it useful to look at some Asthma apps and Breathing apps.
Outpatient clinics
Your child will have regular reviews with the hospital team. The team can include lots of different health professionals. How often the reviews happen depends on how well your child is.
The review will include:
- height and weight measurement to check growth
- a lung function test to measure how well the lungs are working
- a mucus sample to test for bacteria so your child can get the right antibiotics
- a cough suction if your child is young and can't cough up mucus
- a check on how you're going with physiotherapy techniques and whether they need changing.
A stay in hospital
If your child has a chest infection that is severe or continues for a long time, they may need to go to hospital for 10–14 days to have specialist treatment.
Antibiotics: Your child will have these directly into a vein through a 'drip'. Sometimes your child will have a special drip called a 'PICC line'. This is a long tube which lasts for longer than a 'drip' – it doesn't need replacing regularly.
Chest physiotherapy: A professional physiotherapist will do this twice a day. Sometimes, your child will have extra testing just like they do at outpatients appointments such as:
- lung function testing
- mucus sampling
- chest X-ray.
You can go to the New Zealand Bronchiectasis Foundation website for:
Does your child cough?(external link)(external link) Starship and Asthma Foundation, NZ, 2012
Bronchiectasis action plan(external link)(external link) Northland DHB, NZ
Bronchiectasis – information for families [PDF, 722 KB] Northland DHB, NZ
Bronchiectasis – information for preschools and kindergarten [PDF, 291 KB] Northland DHB, NZ
Bronchiectasis – information for schools [PDF, 291 KB] Northland DHB, NZ
Bronchiectasis action plan from KidsHealth(external link) KidsHealth, NZ
Things you can do include providing your child with:
- regular physiotherapy to keep their lungs clear of mucus
- regular exercise and sport
- a healthy balanced diet
- a smoke free environment – keep them away from any tobacco smoke, especially in a house or car
- a flu vaccine every year
- regular hospital clinic and healthcare provider reviews.
Apps
Brochures
Northland DHB, NZ
Northland DHB, NZ
Northland DHB, NZ
Credits: Content shared between HealthInfo Canterbury, KidsHealth and Healthify He Puna Waiora as part of a National Health Content Hub Collaborative.
Last reviewed:





