If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
COPD flare-ups
Also known as COPD exacerbations
Key points about COPD flare-ups
- A flare-up is when your chronic obstructive pulmonary (lung) disease (COPD) symptoms suddenly get worse, and you are experiencing more shortness of breath or an increase in coughing.
- You should act quickly and follow your treatment plan as soon as you realise your symptoms are getting worse.
- If you don't already have one, be sure to ask your healthcare provider about a COPD action plan.

See your doctor or go to the nearest emergency department immediately if you, or someone you care for, experience the following:
|
- Signs of a COPD flare-up include coughing or wheezing more than usual, producing more phlegm or mucus than usual, a change in the colour and consistency of your phlegm, experiencing more shortness of breath (trouble breathing) than usual and feeling more tired.
- The best way to manage a COPD flare-up is to have a COPD action plan and use your medicines as described in the plan.
- A COPD action plan is a written document that provides you with instructions and information on how to manage your COPD on a daily basis. It also tells you how to recognise and cope with worsening symptoms (exacerbations).
- You can develop your COPD action plan with your healthcare provider and set it up to suit the severity of your COPD and your preferences. Be sure to ask your healthcare provider about a COPD action plan.
A COPD flare-up is when your COPD symptoms become worse suddenly or are particularly severe. A flare-up might be triggered by an infection or there may be no obvious cause. A flare-up is also called an exacerbation.
Each COPD flare-up does long-term damage to your lungs and is a common cause of admission to hospital. It's important to be prepared – to recognise the symptoms of a flare-up and know what to do. Taking action early can prevent worsening symptoms and hospital admission. Read more about COPD.
Signs of a flare-up
- Coughing or wheezing more.
- Finding it harder to breathe than normal – being less able to do any physical exercise or do your usual daily activities.
- Producing more phlegm or mucus.
- A change in the colour and consistency of your phlegm.
- Feeling tired – having less energy.
- Eating less.
The best way to manage a COPD flare-up is to have a COPD action plan and use your medicines as described in the plan.
A COPD action plan is a written document that provides you with instructions and information on how to manage your COPD on a daily basis and also how to recognise and cope with worsening symptoms (exacerbations). You can develop your COPD action plan with your healthcare provider and set it up so that it suits the severity of your COPD and your preferences. At each visit with your healthcare provider you can review the plan and make changes to it as needed. However, having an action plan doesn't replace your healthcare provider. It enables you to start treatment early but you should still arrange to see your healthcare provider as soon as possible. Tell them if your symptoms don’t improve after starting the medicines you keep at home.
Here are 2 examples of COPD action plans, choose the one that suits you.
|
COPD action plan |
Blue card regional COPD action plan |
 (external link)
(external link) |
 [PDF, 355 KB]
[PDF, 355 KB] |
|
|
|
The image below shows what happens to your airways when you have a flare-up and they become inflamed, the muscles in the walls tighten and mucus builds up.
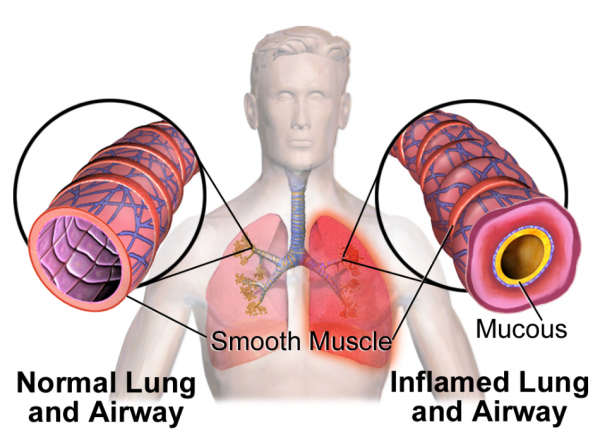
Image credit: Medical Gallery of Blausen Medical 2014 via Wikimedia Commons(external link)
Your action plan will include instructions on changes to make to your medicines when your symptoms get worse. This may include the following:
- Reliever medicine: Increase the dose of your reliever medicine (eg, salbutamol. terbutaline and ipratropium). This quickly opens the airways making it easier to breathe. Relievers usually start working within minutes and their effect lasts for a few hours. Read more about quick relievers.
- Spacer: If you are using a puffer or metered-dose inhaler, use a spacer with it to get the most benefit from your inhaler. Spacers are large empty plastic containers that you attach to your inhaler. By using a spacer with your inhaler, more of the medicine gets into your lungs. They are available free from your doctor. Read more about spacers.
- Steroid tablets: Your doctor may prescribe a course of steroid tablets (prednisone) to take daily for a few days (usually 5 days). They work best if taken as soon as the flare-up starts, so your doctor may give you some tablets to keep at home in case you have a flare-up.
- Antibiotics: Your doctor may prescribe a course of antibiotics if an infection has triggered your flare-up.
Make sure you know all of the medicines you're taking and how to use them correctly. Let your pharmacist or doctor know if you find your inhaler difficult to use. They may be able to find another one that's easier to use.
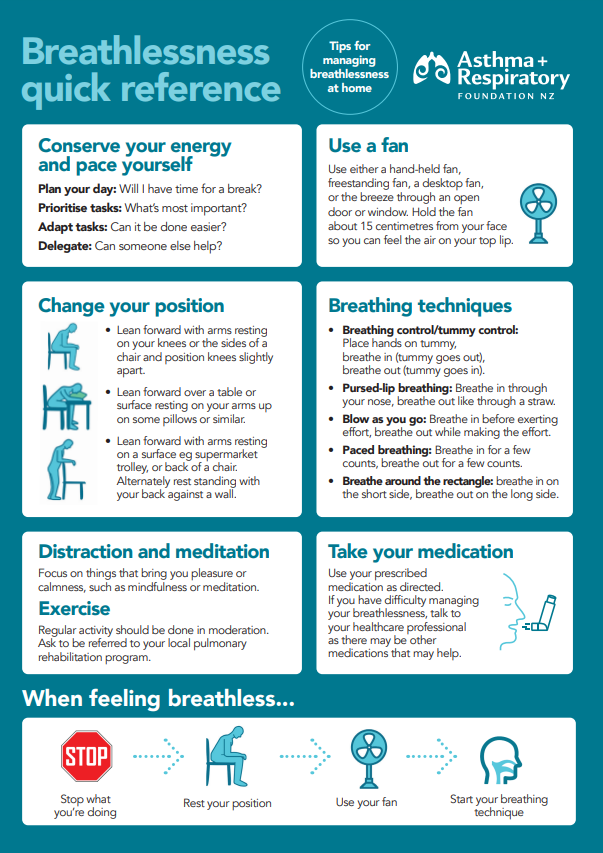
You can also learn these breathlessness strategies(external link) to use, along with making changes to your current medicines, when you're feeling breathless.
Sometimes, you may need to go into hospital if you have a severe flare-up or exacerbation. The table below shows some of the symptoms or signs that may require you to see your doctor or go to the hospital immediately.
See your doctor or go to the nearest emergency department immediately if you, or someone you care for, experience:
|
In the hospital, treatment for a flare-up may include:
- using nebulisers to deliver medicines as a breathable mist if your symptoms don't improve after using inhalers
- oxygen if your oxygen level is low
- a short course of steroid tablets
- antibiotics if you have an infection
- non-invasive ventilation.
Non-invasive ventilation (NIV)
Sometimes, if your COPD flare-up or exacerbation is very severe, you may need a form of breathing support known as non-invasive ventilation (NIV). As its name suggests, NIV is a type of breathing support that is non-invasive. Instead of putting a breathing tube into your airway, it only uses a face mask to support your breathing. This helps remove the excess carbon dioxide in your blood, increases your oxygen levels and reduces the need for being admitted to an intensive care unit (ICU).
Before discharge
Every time you have a flare-up, you're at risk of having another. Before you are discharged from the hospital, your healthcare team will review your medicines and COPD action plan to make sure they are up-to-date. They will also check your inhaler technique and make sure you are using them correctly to prevent the risk of future flare-ups. Sometimes, you may need to attend follow-up clinics with your healthcare provider a few weeks after discharge to make sure you're recovering well. It may take several weeks to get back to your baseline.
It's a good idea to talk about/review what you would like to happen should your COPD get worse. You can kōrero with your hospital doctors and/or your usual healthcare provider. Although it may be hard to talk about, it's important that your healthcare providers and whānau know what your wishes are should you get very sick. Read more about advance care planning.
There are things you can to do reduce the risk of a flare-up. These include learning as much as you can about your COPD, and getting the right help and support to help you manage your condition well.
These include:
- quitting smoking
- exercising daily
- joining a pulmonary rehabilitation programme and going along regularly (ask your healthcare provider if this might be helpful for you)
- getting influenza and pneumonia vaccinations
- taking your COPD medicines daily and regularly, as prescribed by your doctor
- knowing when to next see your doctor.
Read more about self-care for COPD.
Apps reviewed by Healthify
You may find it useful to look at some COPD apps, Breathing apps and Quit smoking apps.
Breathlessness guide and plan(external link) Asthma + Respiratory Foundation NZ
COPD action plan(external link) Asthma + Respiratory Foundation NZ
Apps
COPD apps
Breathing apps
Quit smoking apps
Brochures
COPD breathlessness quick reference guide(external link) Asthma + Respiratory Foundation, NZ
Breathlessness strategies for COPD(external link) Asthma + Respiratory Foundation, NZ
Regional Blue card COPD Action plan [PDF, 355 KB] District Health Boards, NZ
COPD action plan(external link) Asthma and Respiratory Foundation, NZ English(external link), te reo Māori(external link), Samoan(external link), Chinese (simplified)(external link), Tongan(external link)
References
- NZ COPD guidelines 2021(external link) Asthma + Respiratory Foundation, NZ, 2021
- The COPD prescribing tool(external link) BPAC, NZ, 2020
- An update on the pharmacological management of stable COPD(external link) BPAC, NZ, 2020
- Global initiative for chronic obstructive lung disease 2024(external link) GOLD, 2024
Asthma + Respiratory Foundation, NZ, 2021

Asthma + Respiratory Foundation, NZ, 2021
Asthma and Respiratory Foundation, NZ
English, te reo Māori, Samoan, Tongan, Chinese (simplified)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:





