You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Charcot-Marie-Tooth disease (CMT)
Also known as hereditary motor and sensory neuropathy
Key points about Charcot-Marie-Tooth disease (CMT)
- Charcot-Marie-Tooth disease (CMT) is an inherited condition that affects your nerves and muscles.
- Symptoms usually start between the ages of 5 and 15 years, but can start later in life.
- CMT affects your feet and legs first, then later your hands and arms, and the symptoms get worse over time.
- Unfortunately, there’s no cure for CMT, but treatment aims to reduce symptoms and help you manage your daily activities.

Charcot-Marie-Tooth disease (CMT) is an inherited condition that affects your nerves and muscles.
Symptoms usually start between the ages of 5 and 15, but can start later in life. CMT affects your feet and legs first, with weakness and muscle wasting, then later your hands and arms. Symptoms get gradually worse over time.
Unfortunately, there’s no cure for CMT, but treatment aims to reduce your symptoms and help you carry out your daily activities.
Charcot-Marie-Tooth disease (CMT) is caused by changes in certain genes that affect the nerves that send information from your brain and spinal cord to and from the rest of your body. If you have CMT, you may have inherited faulty genes from one or both of your parents.
The nervous system in your body consists of the central nervous system (CNS) and the peripheral nervous system (PNS). The central nervous system is made up of your brain and spinal cord. The peripheral nervous system is made up of nerves that carry messages from your brain and spinal cord to other parts of your body and these are the nerves affected in CMT.
The peripheral nerves have motor and sensory nerves. Motor nerves carry messages from your brain and spinal cord to your muscles, telling them to contract. Sensory nerves carry stimuli such as touch and pain in the form of signals to your brain and spinal cord.
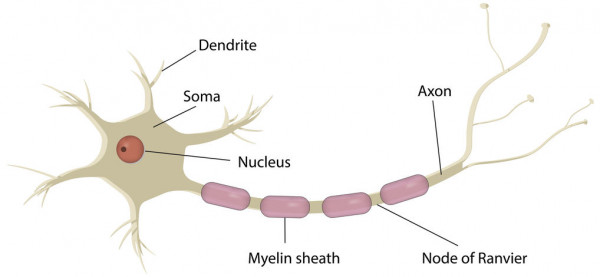
Image credit: 123rf
The structure of a peripheral nerve can be seen in the image above. The axon is similar to the wiring of an electric cable that transmits messages between your brain and spinal cord and the rest of your body. The myelin sheath wraps around the axon and acts as a protection layer, similar to the insulation of a cable, to make sure electrical messages aren’t interrupted while they’re being sent. With CMT, the myelin sheath and axon of peripheral nerves are damaged due to mutations (changes) in certain genes.
There are many different types of CMT that are caused by different faulty genes. The main types of CMT include:
- CMT 1 – this is the most common form of CMT
- CMT 2
- CMT 3
- CMT 4
- CMT X.
Read more about the types and classification of CMT(external link).
The symptoms of Charcot-Marie Tooth disease (CMT) are different for each person and depend on the type of CMT you have.
As it's a progressive condition (that is, symptoms get worse over time), it's sometimes difficult to spot symptoms and diagnose a child with CMT.
Early symptoms of CMT in children include:
- clumsiness
- walking difficulty
- foot drop
- difficulty lifting their feet up from the ground.
Symptoms usually start to appear between the ages of 5 and 15 years, but may not develop until middle age or later.
Common signs and symptoms of CMT include:
- muscle weakness in the lower legs (feet, ankles and legs) at first
- muscle wasting in the lower legs leading to an 'inverted champagne bottle' appearance
- high-arched feet (also called pes cavus), or flat feet
- hammertoes or curled toes (middle joint of the toe bends upwards)
- foot drop causing high lifting of the knees when walking to avoid tripping (also called high stepping gait)
- walking difficulty
- loss of sensation in arms and feet
- spinal deformity, eg, thoracic scoliosis
- cold hands and feet
- muscle and joint pain
- tiredness and fatigue.
As symptoms get worse, it starts to affect your hands and arms more. It then causes problems with daily activities such as buttoning your clothing. Sometimes, damaged nerves can also cause shooting or burning nerve pain, which is also known as neuropathic pain.
See your healthcare provider if you or someone you care for has any of the above symptoms.
Your healthcare provider will ask questions related to your symptoms, including when your symptoms started and if you have any family history of Charcot-Marie-Tooth disease (CMT). They will also examine your legs and arms and test your muscle movements.
If your healthcare provider thinks you may have CMT, you’ll be referred to a neurologist (a doctor who specialises in nervous system conditions) for further testing and treatment.
Tests or investigations you may have include the following:
- Nerve conduction test – this is to test the strength and speed of electrical signals or messages transmitted through your nerves. The signals will be weak and slow if you have CMT.
- Electromyography (EMG) – this measures the electrical activity in your muscles.
- Genetic testing – you'll have blood samples taken to test for faulty genes to confirm and find out which type of CMT you have.
- Nerve biopsy – a sample of your nerve is taken to find out changes in the shape of the nerve under the microscope. This is usually done under a local anaesthetic.
If you have a family history of CMT and are planning to get pregnant, ask your healthcare provider for a referral to a genetic counsellor or specialist for advice. A genetic counsellor or specialist can go through the decision-making process with you and explain the tests and options you may want during pregnancy.
There's no cure for CMT so treatment aims to reduce your symptoms, prevent complications such as joint deformities and falls, and help you manage your daily activities.
You may have a team of healthcare providers involved in your care such as a physiotherapist, an occupational therapist, a podiatrist, an orthotist (a health professional who makes and fits braces and splints), an orthopaedic surgeon, your healthcare provider and a neurologist. You may also need to attend regular follow-ups, depending on the severity of your condition.
Treatment can be categorised into the following areas:
Physiotherapy
Physiotherapy can help improve the symptoms of CMT and reduce the risk of muscle contractures, which happen when a muscle becomes tight and can’t relax or stretch properly. It can also help strengthen your muscles and help with posture and balance issues. Not all people with CMT have the same problems, so ask your physiotherapist for a personalised exercise programme.
Occupational therapy
Occupational therapy helps to improve your daily functioning and activities, eg, dressing, cooking, writing, buttoning and other daily tasks that involve movements of your arms and hands.
Orthoses and walking aids
Orthoses are devices that are worn inside your shoes to help improve how you walk and correct deformities of your feet and legs. There are different devices available, such as ankle or leg braces. Ask your orthotist for one that’s suitable for you.
Pain control
In CMT, there are 2 types of pain:
- Joint and muscle pain – this type of pain can be relieved by regular painkillers such as non-steroidal anti-inflammatory drugs (NSAIDs), eg, ibuprofen.
- Neuropathic or nerve pain – regular painkillers don't usually work for nerve pain. Medicines that have been found to be more effective in relieving nerve pain include amitriptyline, nortriptyline, gabapentin, pregabalin or carbamazepine.
If your pain doesn't respond to one option, your healthcare provider may suggest changing to another or combining more than 1 medicine. Your prescriber will start you on a low dose and gradually increase the dose until you notice an effect.
Surgery
Sometimes, surgery may be needed to correct serious deformities (eg, in your feet, hands or spine) caused by CMT. Your neurologist or healthcare provider will let you know whether you need surgery.
If you have Charcot-Marie-Tooth disease, there are things you can do to take care of yourself.
- Have a good balanced diet and stay at a healthy weight to avoid putting unnecessary strain on your joints and muscles.
- Take good care of your feet with regular cleaning and checking for skin lesions – there's a higher chance of injury and infection when you have loss of sensation in your feet. Read more about foot care.
- Avoid too much alcohol, caffeine and nicotine.
- Avoid medicines that can cause nerve damage – ask your pharmacist or healthcare provider for a list of medicines to avoid if you are unsure.
Apps reviewed by Healthify
You may find it useful to look at some pain management apps, physiotherapy and exercise apps and falls prevention apps.
Charcot-Marie-Tooth disease (CMT) is a progressive condition, meaning that symptoms gradually get worse over time.
Generally, the outlook depends on the type of CMT that you have. For example, most people with CMT1A have a normal life expectancy and little disability, but this can vary from person to person. More severe forms of CMT are associated with major nerve and muscle problems and reduced life expectancy.
Living with CMT can be difficult and challenging both physically and mentally. Talk through your feelings with your family and friends to get the support you need.
CMT NZ(external link) is an online support group on Facebook for people who have been diagnosed with CMT to share experiences and knowledge about the disease. There's also a face-to-face CMT group that meets once a month in Christchurch. Phone 03 354 3943 or email [email protected] to find out more.
Muscular Dystrophy NZ(external link) provides services and support, including a Facebook page, for people affected by neuromuscular conditions, including CMT.
The following links provide further information on Charcot-Marie-Tooth disease. Be aware that websites from other countries may contain information that differs from Aotearoa New Zealand recommendations.
Charcot-Marie-Tooth(external link) Muscular Dystrophy NZ
Charcot-Marie-Tooth disease(external link) Muscular Dystrophy UK
Charcot-Marie-Tooth disease(external link) NHS, UK
Brochures
CMT – a practical guide [PDF, 3.7 MB] Charcot-Marie-Tooth, UK, 2014
Apps
Pain management apps
Physiotherapy and exercise apps
Falls prevention apps
References
- Charcot-Marie-Tooth (CMT)(external link) Muscular Dystrophy NZ
- CMT – a practical guide [PDF, 3.7 MB] CMT UK
- Charcot-Marie-Tooth disease(external link) NHS, UK, 2022
- Charcot-Marie-Tooth disease(external link) Patient Info Professional, UK, 2021
Clinical resources
Charcot-Marie-Tooth disease(external link) Patient Info Professional, UK, 2021
Charcot-Marie-Tooth disease – management and prognosis(external link) UpToDate, 2024
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: New Zealand Rheumatology Association
Last reviewed:





