Bursitis
Key points about bursitis
- Bursitis is a type of inflammation that affects your joints, causing them to be painful, red and swollen.
- It commonly affects your feet, shoulders, elbows, knees and hips. However, you can get bursitis in any joint.
- Inflammation occurs with repetitive movement, pressure on your joint, gout or rheumatoid arthritis, an injury or an infection near or in your joint.
- Symptoms of bursitis include painful, red, hot, swollen joints with some stiffness.
- Bursitis is not usually serious and can be treated with self-care measures at home.

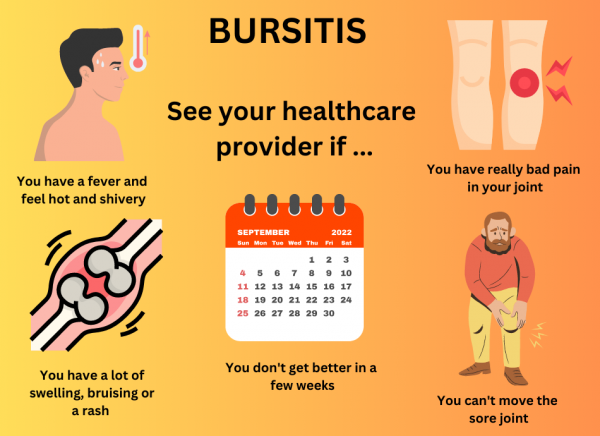
Image credit: Healthify, NZ
There are fluid-filled sacs that sit around your joints to help protect the tissues that slide over your bones when you move. These fluid-filled sacs are called bursa (singular) or bursae (plural). There are over 150 of these in your body but you will unaware of them. They act as lubricants for your bones and soft tissues around them and help reduce friction when you move your joint. Bursitis is the inflammation of these bursae.
They can get inflamed due to:
- repetitive movement of a certain joint, such as when you kneel a lot with work or hobbies, eg, carpet fitters, cleaners and carpenters
- too much pressure on your joint, such as leaning on your elbows to work or study
- gout or rheumatoid arthritis
- an injury near your bursa
- an infection from your skin or near your joint.
Bursitis commonly affects your feet, shoulders, elbows, knees and hips. However, you can get bursitis in any joint.
Common types of bursitis include:
- subacromial bursitis – this causes shoulder pain
- olecranon bursitis – this causes elbow pain and is also known as student's elbow
- prepatellar bursitis – this causes knee pain and is often called housemaid's knee
- greater trochanteric pain syndrome – this causes hip pain
- Achilles heel bursitis – this is found in athletes
- septic bursitis – this is caused by a bacterial infection and may occur in any joint.
Your doctor will ask you questions about your joint pain and work or hobbies that make you more likely to get bursitis. They will also ask whether you have any other medical conditions such as gout or rheumatoid arthritis and check whether you have other symptoms.
Your doctor will also examine your joints. They may also send you for an x-ray or ultrasound scan, order blood tests or take a sample of fluid from your joint swelling using a needle, depending on what they think is the cause. Taking a fluid sample can help diagnose infection or gout arthritis.
You can usually help treat bursitis yourself at home by the following self-care measures.
- Rest as much as you can and avoid pressure, activities or repetitive movement that worsen the symptoms of your affected joint. However, don't stop moving the joint completely as you could lose muscle mass and get long-term stiffness in your joint.
- Use ice to help reduce swelling in your joint and ease pain. You can wrap some ice or an ice pack in a towel and place it on your affected joint for 10–20 minutes. Repeat every few hours during the day.
- Take pain relief medicines such as paracetamol or non-steroidal anti-inflammatory medicines (NSAIDs) such as ibuprofen. Ask your GP or local pharmacist to find out whether it is safe for you to take NSAIDs.
- Use pads and cushions to help protect your affected joint.
- Wear comfortable, supportive shoes. Shoe inserts may also be helpful.
- Lose weight if appropriate.
You may need to see your doctor if your bursitis is caused by an infection, as antibiotics are needed to treat that.
Other treatments of bursitis include the following:
- Orthotics – special devices designed to protect a joint.
- A steroid injection – some types of bursitis can be treated by injection with steroids into your affected joint to help reduce inflammation, but not all types of bursitis can be treated with this. This is usually done shortly after fluid has been removed.
- Physiotherapy – a physiotherapist can teach you suitable exercises to improve your joint movements and strengthen the muscles and soft tissues that support your joints to prevent injuries. Ask your doctor to find out whether you need to be referred to a physiotherapist or find a private physiotherapist here.
- Surgery – surgery is rarely needed to remove your bursa unless you keep getting bursitis.
See your healthcare provider if you experience the following:
- your symptoms don't improve or get worse after self-care measures for a few weeks
- you have a high temperature or fever, and you feel hot and shivery
- you can't move your affected joint
- you have very severe pain in your joint
- you have significant swelling, bruising or a rash over the affected joint.
Apps reviewed by Healthify
You may find it useful to look at some Joint and bone health apps.
Bursitis should go away in a few weeks with self-care measures. See your doctor if your symptoms have not improved and are getting worse after treating it yourself.
You can prevent bursitis by:
- maintaining good posture
- maintaining a healthy weight or losing weight if you are overweight
- making sure any wound is clean if you have any cuts on your skin near a joint
- avoiding repetitive movements and taking frequent breaks, especially if hobbies or work require the same repetitive movements for long periods
- warming up properly before exercising or playing sports
- using pads or cushions to support your joints if you are putting a lot of pressure on them
- avoiding positions that cause pain
- using a dolly or wheeled cart when carrying heavy loads
- using your knees when lifting
- treating any underlying condition affecting your bursitis.
Remember: If it hurts, don’t do it.
The following links provide further information about bursitis. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Bursitis(external link)(external link) HealthInfo Canterbury, NZ
Bursitis(external link)(external link) NHS, UK
Bursitis(external link)(external link) Versus Arthritis, UK
Apps
References
- Bursitis(external link)(external link) HealthInfo Canterbury, NZ
- Bursitis(external link)(external link) NHS, UK
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Bryan Frost, FRNZCGP, Morrinsville
Last reviewed:
Page last updated:





