Broken wrist
Key points about a broken wrist
- A broken wrist is the fracture (break) of any bone in your wrist and is usually due to falling onto your outstretched hand.
- Common symptoms include severe pain, swelling or bruising, tingling or numbness of your hands or fingers, and difficulty moving your hands.
- A broken wrist is usually diagnosed with an X-ray but the break is sometimes difficult to see.
- Treatment aims to put the broken bones back together so the bone can heal properly and you get back normal movement of your wrist.
- For minor breaks, you will need to wear a cast or splint. Major breaks may require surgery.

A broken wrist is the fracture (break) of any bone in your wrist and usually happens after falling onto your outstretched hand.
Wrist fractures are more common for children and young adults, especially if they take part in high-risk activities. They also become more common as you get older as your bones get less strong (osteoporosis) and you’re more likely to fall.
Common symptoms of a broken wrist include severe pain, swelling or bruising, tingling or numbness of your hand or fingers, and difficulty moving your hand.
You are likely to need an X-ray to diagnose a broken wrist but the break is sometimes difficult to see.
Your wrist joint is made up of several bones. These include 8 carpal bones and the radius and the ulna, which are the long bones in the lower part of your arm (see the image below). Any of these bones can break. However, the more common wrist fractures include:
- the ends of the radius or ulna
- the scaphoid bone – one of the carpal bones in your wrist.
A broken wrist usually happens after you've fallen onto an outstretched hand, eg, if you trip and stretch your arm out to try and break the fall. Other causes include:
- serious accidents such as motor vehicle accidents
- a break that occurs in a weak bone, eg, if you have osteoporosis.
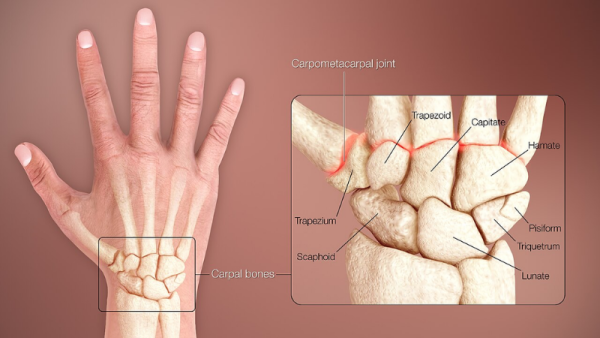
Image credit: Scientific Animations via Wikimedia Commons(external link)
If you think you or someone you care for has a broken wrist, you should:
- go to the nearest emergency department or call 111 if it's badly broken or if you have numbness in your fingers
- see your healthcare provider or an accident and urgent care clinic if it’s a less severe break
- stop using, or avoid moving, the injured arm as much as possible
- if there's any bleeding, apply pressure to stop it using a clean pad or dressing
- ice the injured area using an ice pack or a bag of frozen peas wrapped in a clean towel
- remove any jewellery, such as rings or watches, as your hand, wrist or fingers could swell up
- avoid eating and drinking in case you need surgery to fix the broken bone.
Apps reviewed by Healthify
You may find it useful to look at some first aid and emergency apps.
Your healthcare provider will assess your general condition, and how serious your injury is. They’ll ask about how the injury happened, any symptoms you have and your medical history.
The most common way to diagnose a fracture is with an X-ray. This will show the type of break and its location within the bone. Sometimes, a wrist fracture is hard to see on an X-ray. In that case, you may need another X-ray after a week or more, or a CT scan or MRI scan.
The aim when treating a broken wrist is to put the broken bones back together so that the bone can heal properly and you get normal movement of your wrist back.
The treatment you receive depends on how bad the break is. Other factors that affect your treatment include:
- the type of fracture
- your age
- whether any parts of the bone(s) have moved out of place
- whether the overlying skin is broken or any bones have broken through your skin
- the number of bone fragments resulting from the fracture
- your job or usual activities.
If you have a minor fracture, you’ll usually be fitted with a cast or splint to hold your bone(s) together and support your wrist while it heals.
If you have a more serious fracture where parts of the bone have moved out of place, a doctor will try to return the broken parts to their normal position, either manually using their hands or through surgery to insert pins, plates or screws to hold your bone(s) in place. In both cases you’ll be given pain relief medicine and be advised about care following treatment. This may involve physiotherapy or hand therapy.
If your fracture happened after a minor incident, such as a fall from standing height, you may be assessed for osteoporosis. Osteoporosis is a condition where your bones are thinner and weaker than normal, which means they can break easily. Read more about osteoporosis and preventing falls.
There are several things you can do to help the recovery of your broken wrist. For example:
- Take regular pain relief medicines if you have any pain.
- Keep your hand raised above your elbow whenever possible to reduce swelling – you can use a pillow at night for this. You can use your hand for light activities such as eating, writing, typing, dressing yourself, using your cell phone and folding laundry.
- Do gentle exercises for your shoulder, elbow, fingers and thumb, as advised by your healthcare providers to reduce stiffness and swelling.
- Avoid heavy lifting or activities that need your wrist to work hard until you've been told it's okay to do so.
- Position your arm with your thumb up rather than letting your arm rest with the palm down all the time as this will help with later stiffness.
- Keep your cast dry, you can wrap your arm in a plastic bag when you have a shower.
- Even if it gets itchy, don't use anything to scratch under your cast as this could break the skin and lead to infection.
- A sling isn't usually needed for a wrist fracture, but if you've been given one, use it as little as possible and take it off when doing your exercises. This will stop your shoulder and elbow getting stiff.
Read more about exercises for your arm and hand while in a cast(external link) and care of your broken wrist after the cast's been removed(external link).
Apps reviewed by Healthify
You may find it useful to look at some hand and wrist exercise apps.
If you have a cast, you’ll need to wear it until your bones heal. This will usually take 4 to 6 weeks, or longer if your fracture is more serious.
You may be given a splint to wear after the cast is taken off. A splint can help with comfort and gives you some support until you feel confident to use your hand again.
If you’ve had surgery and the bones are well fixed with a plate and/or screws, you might not have a cast or you might have one for a shorter time (10 to 14 days). After that you may wear a splint some or all of the time for 3 to 4 weeks. However you will be able to start moving your wrist, usually under the guidance of your surgeon and/or physiotherapist or hand therapist. If your fracture was caused by an injury, ACC(external link) may also be able to provide support for your recovery.
Don’t expect your hand and wrist to be normal as soon as the cast comes off as it can take a while for the stiffness to wear off. Eventually, your hand and wrist will work well again, but it’ll take time.
The following links provide further information about broken wrist. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Brochures
Care of your wrist and hand following a fracture(external link) HealthInfo Canterbury, NZ
Exercises of your arm and hand while in a cast(external link) HealthInfo Canterbury, NZ
Apps
References
- Wrist fractures in adults(external link) Auckland Regional HealthPathways, NZ, 2021
- Wrist fractures(external link) Patient Info, UK, 2024
- Broken arm or wrist(external link) NHS, UK, 2023
- Distal radius fractures (broken wrist)(external link) OrthoInfo, US, 2022
Brochures

Exercises of your arm and hand while in a cast
HealthInfo Canterbury, NZ

Care of your wrist and hand following a fracture
HealthInfo Canterbury, NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Grace Lee, FRNZCGP and Clinical Educator
Last reviewed:





