Common causes of bleeding after vaginal sex
Cervical polyps
Polyps are small swellings in the linings of open spaces in your body. They can occur in many parts of your body, such as your uterus, nose or bowel, and are usually not serious.
It’s common for polyps to grow on your cervix. The surface of polyps is not tough like skin, so if they’re rubbed during sex they can bleed.
Read more about cervical polyps.
Cervical ectropion
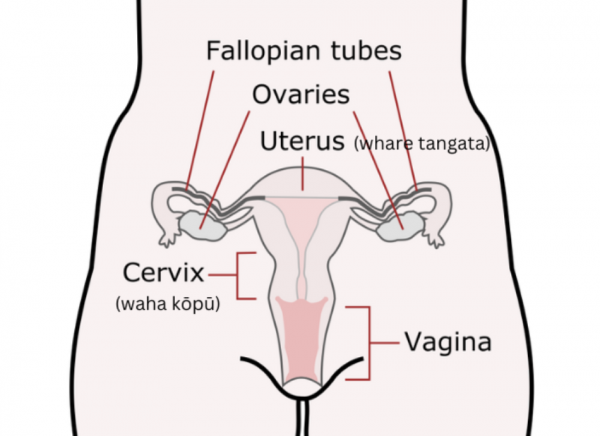
This condition isn't serious but is one of the more common causes of bleeding after sex. Sometimes female hormones cause the more fragile cells inside your cervical canal (the inner part which connects your uterus to your vagina) to grow onto the outer part of your cervix (the part at the top of your vagina). This is why you sometimes get bleeding after a cervical sample has been taken (smear).
The cells haven’t grown too much and are not abnormal, they're just in the wrong place on the outside part of your cervix, where they can be damaged during sex. Read more about cervical ectropion.
Thrush
Occasionally a bad case of thrush (candida) can cause bleeding. Usually, there will be a lot of discharge and discomfort as well. You can buy treatment for thrush over-the-counter at a pharmacy. If you treat thrush but the bleeding doesn’t go away, or if you get thrush often, see your healthcare provider for a check-up. Read more about thrush.
Bleeding due to hormonal contraception
When you first start taking hormonal contraception you can have some irregular bleeding which can last for months. This includes oral contraceptive pills (the pill and mini pill), contraceptive injections (depo), implants and intrauterine devices (IUDs). This irregular bleeding can happen after sex. Usually it goes away with time but if it doesn’t, see your healthcare provider to decide if you need to change to a different type of contraceptive. Read more about contraceptive options.
Bleeding caused by sex
Occasionally, sex can cause bleeding from your vagina or vulva. This can happen sometimes the first time you have sex. Any bleeding shouldn't be heavier than a period or last more than a couple of days. Read more about hymens and virginity.
If there's a graze (abrasion) on your vulva there can be spots of bright blood on your underwear or toilet paper which quickly stops. The skin will be tender (sore to touch) too, and you might be able to see it with a mirror. This can be caused by masturbation or sex toys as well as intercourse.
Although sex doesn’t usually cause damage to your vagina, a rip or tear in your vagina can sometimes happen. Your vagina has a lot of blood vessels just under the surface, so the bleeding can be very heavy – if so you’ll need to go to hospital.
Bleeding from your vagina after sex is more common if you have gone through menopause and stopped having periods.
- This is often associated with a condition called atrophic vaginitis (also called genitourinary syndrome of menopause) where the lining of your vagina becomes thinner and more vulnerable to infection. Read more about atrophic vaginitis.
- Women on medications for breast cancer (such as tamoxifen) may also have this condition due to low hormone levels. Using a water-based lubricant during sex can help prevent bleeding if this is the cause.
Read more about menopause.
Less common but more serious causes of post-coital bleeding
Cervical cancer
Cervical cancer is a serious condition but if it's treated early it can be cured completely. Fortunately, this cancer can be found through cervical screening tests before it becomes a serious threat.
Cervical screening is a very effective way of preventing cervical cancer. The chance of getting cervical cancer if you have regular screening is very very low. However, no test is perfect, so even if you've had a recent cervical screening test, you should still see your healthcare provider if you have post-coital bleeding. Read more about cervical screening and cervical cancer.
Rarely, vaginal cancers or endometrial cancer can cause bleeding after sex, but they will usually cause bleeding at other times as well.
Cervical infection
Infection of your cervix is usually a sexually transmitted infection (STI). Some STIs, such as chlamydia and gonorrhoea, are serious and need to be treated. The infection can spread from your cervix to your uterus and fallopian tubes and cause pelvic inflammatory disease or problems getting pregnant. Because they are sexually transmitted, your sexual partner/s will also need to be checked for infection.
Pregnancy
Bleeding in early pregnancy is common. Most people will know they’re pregnant soon after missing a period, but others won't realise they’re pregnant for a couple of months. If early pregnancy bleeding occurs around the time you're expecting a period, it's easy to mistake this for a period.
If you have bleeding after sex it’s worth doing a pregnancy test, even if you're using contraception. The treatment of bleeding in early pregnancy is very different to treatment of post-coital bleeding.
It's not normal for girls who haven't started having periods to have vaginal bleeding. See your healthcare provider for advice.
|