The greatest risk factors for endometrial cancer are age and obesity.
- Endometrial cancer is much more common in post-menopausal women, with the average age at diagnosis being 60–65 years.
- Being overweight or obese increases your risk of developing endometrial cancer, with >50% of endometrial cancers being attributed to obesity. See the FAQ section below for further information.
- Having endometrial hyperplasia (pre-cancerous condition, where the lining of the uterus is thickened) also increases your risk.
Other risk factors include:
- Polycystic ovarian syndrome (PCOS) – women with PCOS often have irregular periods and are more likely to become overweight and develop diabetes.
- Type 2 diabetes, hypertension, raised cholesterol.
- Some hormone therapies used for breast cancer therapy such as Tamoxifen can also increase the risk of endometrial cancer.
- If you are prescribed tamoxifen your doctor will discuss this with you and also talk about how this risk can be minimised.
- It is important to remember that the improvement in survival from breast cancer is a big benefit, compared to the small increase in risk of endometrial cancer.
- Hormone producing tumours – this is a rare cause of endometrial cancer.
- Genetic problems such as Lynch syndrome. These are relatively rare (around 5%) but women with Lynch syndrome often develop endometrial cancer before menopause.
- A family history of endometrial, ovarian or colorectal cancer.
as Lynch syndrome. These are relatively rare (around 5%) but women with Lynch syndrome often develop endometrial cancer before menopause.
FAQs about risk factors
Why is endometrial cancer more common after menopause?
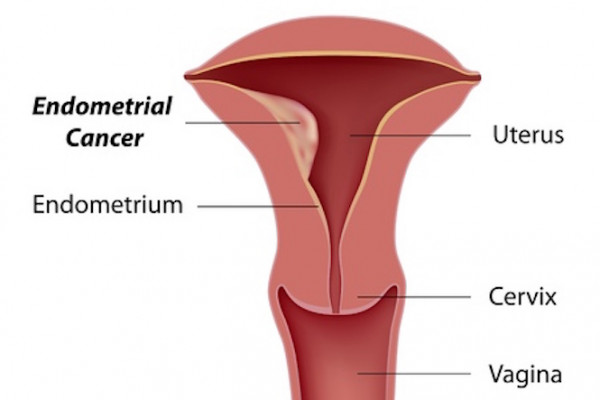
The increased risk of endometrial cancer after menopause is because the lining of the uterus is no longer shed as part of a woman’s period each month.
Having regular periods protects against endometrial cancer because it prevents build-up of the cells lining the uterus. During a normal monthly cycle, endometrial cells lining the uterus grow and mature in response to the hormones oestrogen and progesterone, preparing your womb for implantation and pregnancy. If implantation doesn't occur, these cells are shed and you have your period.
After menopause, oestrogen is mostly made in the body by fatty tissue, and your ovaries are no longer producing hormone-cycles to regulate the lining of the uterus. The enzymes that produce oestrogen increase in quantity and activity with age, increasing the production of oestrogen. This increases the risk of endometrial cancer in post-menopausal women.
Why does being obese increase my risk of endometrial cancer?
It's been estimated that 40% of endometrial cancers are due to obesity.
If you have a BMI of 35, your chance of getting endometrial cancer is 4.7 times the chance of a woman with a BMI of 25. The outcomes for endometrial cancer are also worse for obese women compared to women who are in a healthy weight-range.
Women who are overweight are less likely to have regular periods, and therefore more likely to have an abnormal build-up of endometrial cells (before menopause).
Although oestrogen is usually produced in the ovaries, fat cells also make oestrogen, so women who are overweight generally produce more oestrogen. This stimulates the lining of the uterus to grow, and increases the risk of endometrial cancer. Obesity also creates a chronic inflammatory state in the body, which contributes to increased cancer risk.
How does the pill reduce my risk of endometrial cancer?
The combined contraceptive pill (and hormone replacement therapy) include both oestrogen and progesterone. Progesterone slows cell growth, balancing the stimulating effect of oestrogen, which helps prevent abnormal cell growth and the development of endometrial cancer.