Basal cell carcinoma | Mate pukupuku kiritai
Also known as rodent ulcers
Key points about basal cell carcinoma
- Basal cell carcinomas (mate pukupuku kiritai, BCCs) are the most common and the least serious form of skin cancer – as long as they are treated.
- BCCs are a type of non-melanoma skin cancer.
- They often appear as a pale, pink or pearly smooth lump.
- They're more common among older people, but can develop in younger people.
- Most BCCs are caused by long-term exposure to ultraviolet (UV) radiation from sunlight, so almost all occur on parts of your body that get the most sun.
- They tend to be slow growing and very rarely spread to other parts of your body. Therefore they are almost never a danger to life.

Basal cell carcinomas (BCC) occur when a mutation develops in one of your skin's basal cells. Basal cells are found at the bottom of the epidermis –the outermost layer of your skin. Basal cells produce new skin cells as old ones near the surface die off. Sun exposure is the main cause of damage leading to BCC. As a result, almost all BCCs occur on parts of your body that get the most sun.
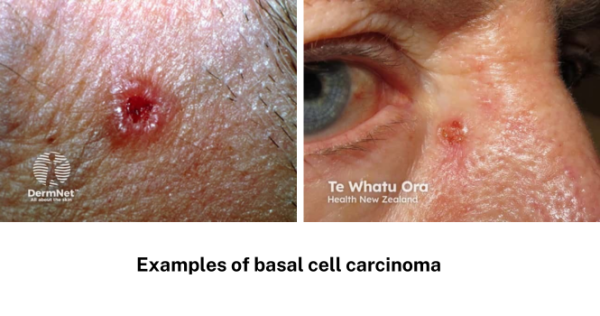
Image source: DermNet
The main cause of damage leading to BCC is sun exposure. This is usually a combination of:
- long-term, everyday sun exposure, and
- occasional intense exposure, usually leading to sunburn.
In some cases, they are the result of damage caused by things such as burns, scars, infections, vaccinations or tattoos.
You are at highest risk of developing a BCC if you:
- are older
- have pale skin and burn easily
- have spent a lot of time outdoors for work or leisure
- live in a sunny climate
- use sunbeds or sunbathe
- have previously had a basal cell carcinoma or another type of skin cancer
- have a condition or take medicines that affect your immune system (immune suppression).
Almost all BCCs occur on parts of your body that get the most sun, such as your face, ears, neck, scalp, shoulders and back. They occur less often on other parts of your body or legs. In rare cases, they can appear on parts of your body that are normally protected from the sun.
BCCs often appear as a change in your skin, such as a lump or a sore that does not heal.
The main features are:
- slow growing – months to years
- a pearly white, skin-coloured or pink bump that is translucent (you can see a bit through the surface)
- waxy, small, raised lesions that may have a dent in the centre
- brown or blue-black areas, in some cases
- a scaly red flat mark on the skin, in some cases
- a tendency to bleed or turn into an ulcer
- scaly, oozing or crusted areas
- varying in size from a few millimetres to several centimetres in diameter.
Apps reviewed by Healthify
You may find it helpful to look at the DermDiag app.
If you notice a change to or growth on your skin, make an appointment to see your doctor straight away. Your doctor will assess the size, location and look of the growth. They will also ask you how long you have had it, whether it bleeds or itches, etc.
If your doctor thinks the growth may be cancer, they may take a small sample of tissue (a biopsy). The tissue sample will be sent to a laboratory and examined under a microscope. Your doctor will let you know whether the sample showed any cancer cells, and will recommend appropriate treatment if necessary.
Treatment of basal cell carcinoma depends on its type, size and location and other factors, such as your preference.
Options include:
- surgical removal of the cancer (this is the most common treatment method)
- freezing it with liquid nitrogen
- topical therapies (creams)
- radiotherapy
- photodynamic therapy (a specialist treatment using light to activate creams).
If you have a BCC, talk with your doctor about which treatment option is best for you. Treatment will almost always cure a BCC, provided it is found at an early stage. Your doctor may want to plan a future appointment to check for recurrences, new skin cancers or precancerous changes.
Read more about skin cancer treatment.
Most basal cell carcinomas can be treated and cured. However, it is possible for these types of cancers to recur or for new skin cancers to appear.
Do the following to reduce the risk of new cancers occurring:
- Keep all follow-up appointments with your GP or skin specialist.
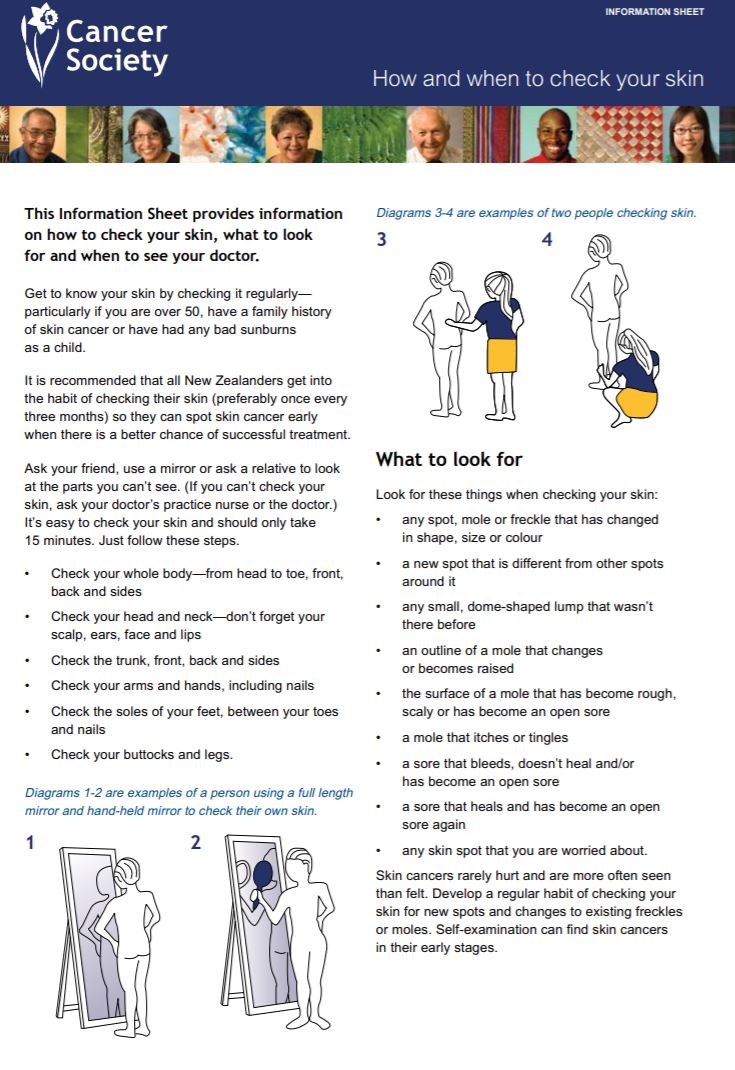
- Regularly check all your skin (from head to toe). If you see anything that is growing, bleeding or in any way changing, go and see your doctor straight away.
- Protect your skin from the sun and avoid indoor tanning. This is essential to prevent further damage, which will increase the risk of getting another skin cancer.
Ways to protect your skin
- Avoid outdoor activities when the sun is strongest – between 10 am and 4 pm from September to April in Aotearoa New Zealand.
- Wear sunscreen and lip balm daily that offer SPF 30 or higher sun protection.
- Use sunscreen that offers broad-spectrum (UVA/UVB) protection and is water resistant.
- Apply the sunscreen and lip balm to dry skin 15 minutes before going outdoors.
- Apply the sunscreen to every part of your body that will not be covered by clothing. Reapply it every two hours if you are swimming or sweating.
- Whenever possible, wear a wide-brimmed hat, long sleeves and long pants.
- Wear sunglasses to protect the skin around your eyes.
- Avoid getting a tan and never use a tanning bed or sun lamp.
See more information on sun safety.
Apps reviewed by Healthify
You may find it useful to look at some Sun safety apps.
Basal cell carcinoma(external link) DermNet NZ
Basal cell carcinoma(external link) Skintel, NZ, 2022
Apps
Brochures
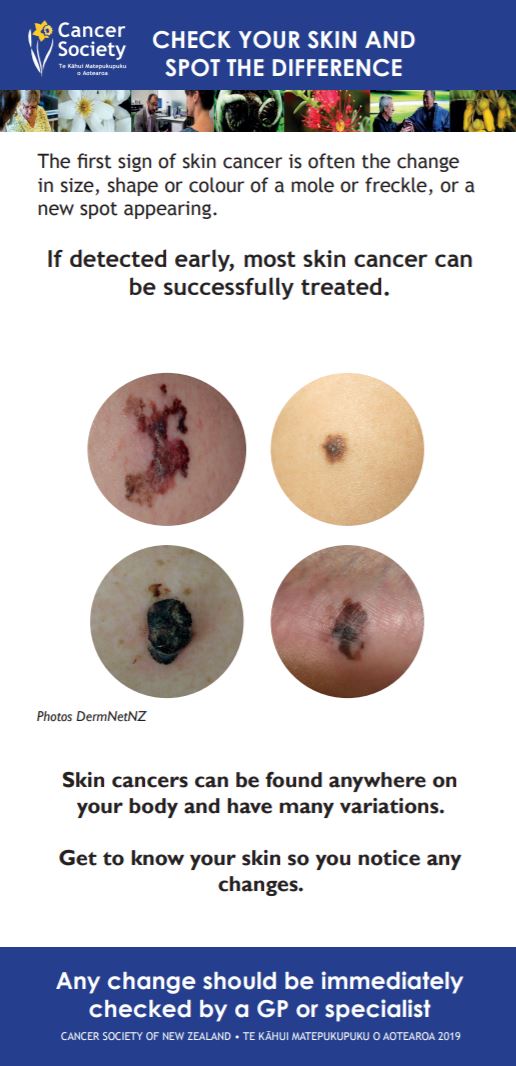
Check your skin and spot the difference(external link) Cancer Society, NZ, 2019 English and te reo Māori
Basal cell carcinoma patient information sheet(external link) British Association of Dermatologists
References
- Telfer NR, Colver GB, Morton CA. Guidelines for the management of basal cell carcinoma(external link) Br J Dermatol. 2008;159:35–48.
- Skin lesion excision(external link) Auckland Regional HealthPathways, NZ, 2020
Video: Goodfellow Unit MedTalk: Non-melanoma skin cancers
Dr Diana North, Goodfellow GP Advisor talks with Dr Marcus Platts-Mills, Dermatology and Skin Cancer Surgery specialist, about the management of non-melanoma skin cancer in primary care.
(Goodfellow Unit, NZ, 2017)
See our page Skin cancer for healthcare providers
Resources
Managing non-melanoma skin cancer in primary care – a focus on topical treatments(external link) BPAC, NZ, 2013
Guidelines for the management of basal cell carcinoma(external link) British Association of Dermatologists
Clinical practice guidelines for keratinocyte cancer(external link) Cancer Council, Australia, 2019
Brochures
Cancer Society, NZ, 2019
Cancer Society, NZ, 2010
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Alice Miller, FRNZCGP, Wellington
Last reviewed:
Page last updated:





