Autoimmune diseases overview
Key points about autoimmune diseases
- Autoimmune diseases are conditions in which your immune system mistakenly attacks your own cells causing damage to organs in your body.
- Different autoimmune diseases affect different parts of your body, so symptoms depend on which type of autoimmune disease you have and how it affects your body.
- Examples of autoimmune diseases are Coeliac disease, Crohn’s disease, lupus and rheumatoid arthritis.
- Most are long-term conditions and symptoms may come and go over time.
- Autoimmune diseases can't be cured, but there are treatments to help you manage your symptoms and slow down the progression of the disease.

A normal immune system helps you fight off harmful things such as infections, by killing bacteria or viruses that get into your body.
If you have an autoimmune disease, your immune system attacks your own healthy cells. This causes damage to different parts of your body depending on the areas that are affected.
Examples of autoimmune diseases include those that affect your:
- gut, eg, coeliac disease, Crohn's disease, ulcerative colitis
- joints, eg, rheumatoid arthritis, psoriatic arthritis
- pancreas, eg, type 1 diabetes
- thyroid gland, eg, Graves' disease
- nervous system, eg, Guillain-Barre syndrome, multiple sclerosis, myasthenia gravis
- skin, eg, psoriasis
- blood, eg, pernicious anaemia.
There are also autoimmune diseases that can affect many parts of your body, eg, lupus, scleroderma and Sjögren’s syndrome (this mainly affects your salivary and tear glands).
You can have more than 1 autoimmune disease at a time.
Most autoimmune diseases are chronic (long-term) conditions and symptoms might come and go over time. Generally autoimmune diseases don't affect how long you'll live.
It's not clear why some people get autoimmune diseases, but there often appears to be a genetic predisposition. This means you have a higher chance of getting the condition if other members of your family also have it.
You also have a greater chance of getting a different autoimmune disease if a relative has an autoimmune disease, eg, one sibling (sister or brother) may have type 1 diabetes while another has coeliac disease. You can also have more than one autoimmune condition.
If you have certain genes, at some stage something in your environment may trigger the symptoms of an autoimmune condition. These factors include:
- an infection
- stress
- medicines
- diet
- UV radiation.
In general, autoimmune conditions are more common in women than men. Some autoimmune diseases are more common in certain ethnicities. Other factors such as smoking, your diet and being very overweight can increase your risk of developing autoimmune disease.
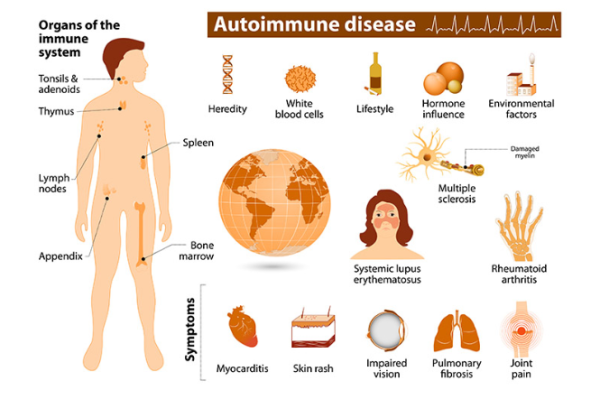
Image credit: NIEHS via Wikimedia Commons(external link)
The symptoms you have will depend on the parts of your body that are affected by the autoimmune disease that you have. For example, coeliac disease damages your small intestine so you may have gut symptoms such as diarrhoea (runny poo) or tummy pain.
As well as symptoms that are specific to your autoimmune condition, you may also have general symptoms, such as:
- tiredness or fatigue
- fevers
- loss of appetite
- loss of weight
- rash
- a feeling that something's not quite right.
When to see a healthcare provider
It's a good idea to see your healthcare provider if:
- you experience any of these general symptoms often, and without a clear cause
- you have muscle, bone, or joint pain that’s not related to an injury, or pain in lots of areas of your body.
Your healthcare provider will ask you questions about your symptoms and examine you. Depending on what they think is causing your symptoms, they may also order tests to find out the cause. They may then refer you to an appropriate medical specialist, eg, if you have coeliac disease, you’ll see a gastroenterologist, or if you have rheumatoid arthritis you’ll see a rheumatologist.
Autoimmune diseases can be hard to diagnose as the symptoms can come and go. It can be useful to keep a diary of your symptoms over time. You may need to see your healthcare provider more than once to identify the problem.
Currently, autoimmune diseases can't be cured. However, there are treatments that can help you manage your symptoms and slow down the progression of your disease. These may be in the form of tablets or injections. Your treatment will depend on the particular autoimmune condition that you have. Your healthcare provider will advise on the best treatment options for you.
In general, lifestyle changes can significantly help with managing the symptoms of many autoimmune diseases. Consider:
- maintaining a healthy diet and a healthy weight
- getting enough rest and sleep
- exercising regularly in a way that suits you
- reducing stress and getting enough support.
Apps reviewed by Healthify
You may find it useful to look at some nutrition, exercise and weight management apps and mental health and wellbeing apps.
Autoimmune NZ(external link) provides support and resources for people affected by autoimmune diseases. Email [email protected] or phone 021 244 4544. There’s also a private Facebook page.
There are also support organisations for people with different autoimmune diseases. Try searching the name of your condition in the support section on the Healthify website to see what’s available.
The following links provide further information about autoimmune diseases. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Autoimmune diseases – an overview(external link) Health Direct, Australia
Autoimmune diseases(external link) Australasian Society of Clinical Immunology and Allergy, Australia
Autoimmune diseases(external link) National Institute of Environmental Health Sciences, US
Apps
Nutrition, exercise and weight management apps
Mental health and wellbeing apps
References
- Autoimmune diseases – an overview(external link) Health Direct, Australia
- Autoimmune diseases(external link) Australasian Society of Clinical Immunology and Allergy, Australia
- Study offers new clues to why most people with autoimmune diseases are women(external link) NIH, US, 2024
See our page Long-term conditions for healthcare providers
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Sara Jayne Pietersen, FRNZCGP, Auckland
Last reviewed:





