Wishing everyone happy holidays and a joyful New Year from the Healthify team. Don't forget to Slip, Slop, Slap and Wrap!
Psoriatic arthritis
Key points about psoriatic arthritis
- Psoriatic arthritis is a type of chronic joint inflammation.
- It’s related to psoriasis, an autoimmune skin rash with red, scaly patches.
- Common symptoms include joint pain, stiffness and swelling.
- There’s no cure, but treatment can help manage symptoms and improve quality of life.
- Regular self-care and medical management can reduce flare-ups prevent joint damage.

Psoriatic arthritis is a type of inflammatory arthritis linked to psoriasis, a skin condition with red, scaly patches of skin. The tissues around your joints, which are called the synovium, get inflamed causing pain, stiffness and swelling. It can affect any joint, but it’s most common in your fingers, feet, toes, knees and sometimes your spine. Your tendons and ligaments can also get inflamed.
Psoriatic arthritis usually develops in people who already have psoriasis, but it can also appear before the skin rash develops. Up to 3 in 10 people with psoriasis get psoriatic arthritis, usually within 10 years of the psoriasis first appearing. It can happen at any age, most commonly between the ages of 25 and 50. It's equally common in men and women.
The exact cause of psoriatic arthritis is not known. Genes are important because the condition is more likely if someone in your family has it. It’s thought that if you have an increased chance of getting psoriatic arthritis due to your genetic makeup, an environmental factor (such as a virus infection or trauma) may trigger your immune system to mistakenly attack your own tissues, causing inflammation.
Lifestyle factors such as smoking and stress increase your risk as well.
Symptoms can be anywhere from mild to severe. They are different for each person, but commonly include:
- joint pain and stiffness – worst first thing in the morning or after rest
- swelling – sausage-like swelling in entire fingers and/or toes (dactylitis).
- skin rash – red patches with silvery scales (psoriasis).
- nail changes – pitting (tiny dents in your nails), discolouration, or separation from the nail bed.
- fatigue – tiredness which doesn’t get better with rest.
- inflammation of your eyes – conjunctivitis or uveitis.
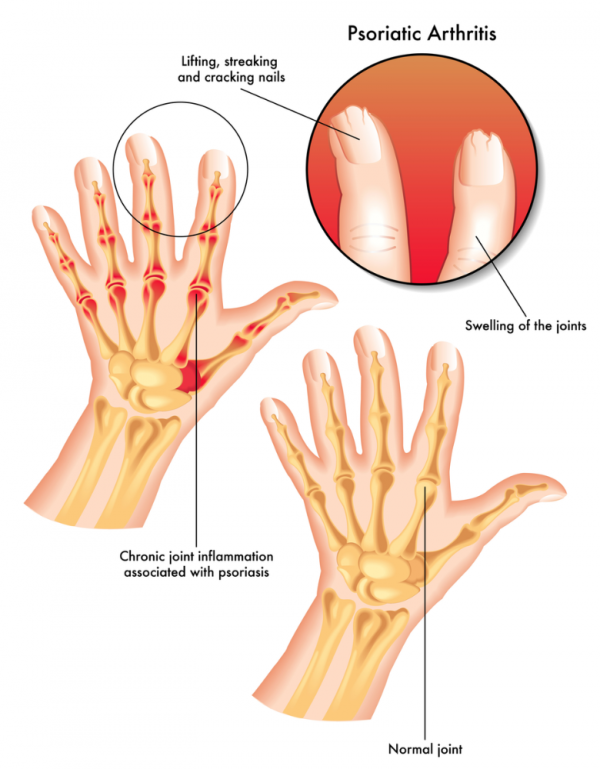
Image credit: Depositphotos
There isn’t a test which shows for certain you have psoriatic arthritis when it first begins. Your healthcare provider will talk with you about your symptoms and medical history and examine your joints and skin. They may do blood tests and X-rays to rule out other types of arthritis.
You may be referred to a rheumatologist, a doctor specialising in joints. What happens with your joints over time can make diagnosis clearer.
Managing psoriatic arthritis includes a mix of treatments and lifestyle changes to protect your joints:
- During a flare-up, rest your joints. Splints can help with this.
- Use heat and cold therapy. Heat can soothe stiff joints, while cold packs can reduce swelling.
- Use paracetamol and/or, if they are safe for you, non-steroidal anti-inflammatory drugs for pain. Be sure to talk to your healthcare provider about whether you should take these kinds of medicines.
- Give up smoking if you're a smoker.
- Try massage.
- Between flare-ups stay active. Regular, gentle exercise helps keep your joints flexible and the muscles around your joints strong enough to support them. Consider low-impact options such as swimming.
- Manage stress – stress can worsen flare-ups, so explore relaxation techniques such as mindfulness or yoga.
Apps reviewed by Healthify
You may find it useful to look at some Psoriasis apps and Quit smoking apps.
Although there’s no cure, treatments can help control symptoms and prevent joint damage.
Medicines
Disease-modifying antirheumatic drugs (DMARDs) are medicines which are taken every day to reduce joint damage. They work by blocking inflammatory chemicals. Examples are methotrexate, leflunomide and sulfasalazine. You need to see a rheumatologist to be prescribed these medicines. They should be started as soon as possible after your psoriatic arthritis diagnosis and can take 2 to 6 months to work. You will need to have blood and urine tests to monitor the effects of these medicines.
Biologics dampen your immune response by targeting specific proteins. Examples are adalimumab, etanercept, infliximab and secukinumab. These medicines are given by injection under your skin or by intravenous infusion through a drip into your vein. These medicines also need to be started by a rheumatologist. Read more about biologics.
Different medicines work better for different people, so you may need to try several before you find the right one for you.
Steroid injections into individual joints can reduce inflammation in flare-ups but shouldn’t be used too many times in the same joint.
Surgery
Joint replacement surgery may be needed if there is significant damage.
Psoriatic arthritis is a long term condition, with recurrent flareups. Some people find each flare-up is similar, but for others it's progressive (gets worse with time). With early diagnosis and regular treatment, most people with psoriatic arthritis can manage their symptoms well and prevent serious joint damage. However, regular check-ups and adjustments to treatment are important to help maintain your quality of life.
Arthritis New Zealand(external link) offer advice for people living with arthritis, call 0800 663 463
Psoriatic arthritis(external link) Psoriasis Association, UK
Brochures
What is psoriatic arthritis? (PSa)(external link) Arthritis New Zealand, 2022
Psoriatic arthritis(external link) Arthritis New Zealand, 2011
Apps
Psoriasis apps
Quit smoking apps
References
- Psoriatic arthritis(external link) Patient, UK, 2024
- Psoriatic arthritis(external link) DermNet, NZ, 2019
- What is psoriatic arthritis? (PSa)(external link) Arthritis New Zealand, 2022
Psoriatic arthritis(external link) Associate Professor Will Taylor, University of Otago, NZ (PPT slides)
Psoriatic arthritis(external link) DermNet, NZ
Brochures
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator.
Last reviewed: