You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Chemotherapy
Key points about chemotherapy
- Chemotherapy is a term used for medicines designed to kill cancer cells or slow their growth.
- Depending on the type of cancer you have, chemotherapy may be a treatment option. It can be used alone or in combination with other treatments such as surgery or radiation.
- Find out about more about chemotherapy and how it is used.

Chemotherapy (also called chemo) is a term for a group of medicines usually used to treat cancer. There are many different types of chemotherapy that work in different ways, so different types and combinations of chemo may be used for different cancers.
Depending on your type of cancer and how advanced it is, chemotherapy can do the following:
- Cure cancer: When chemotherapy destroys cancer cells to the point that they can no longer be found in your body and won't grow back.
- Control cancer: When chemotherapy stops cancer from spreading, slows its growth, or destroys cancer cells that have spread to other parts of the body.
- Ease cancer symptoms: When chemotherapy shrinks tumours that are causing pain or pressure.
Chemotherapy can be used alone to treat cancer, or it can be used with surgery or radiation or other types of medicines.
- Chemotherapy may be started after surgery, when a tumour or most of the cancer is removed. In this way, the chemotherapy kills any cancer cells that weren't removed during surgery.
- In other cases, chemotherapy is given before surgery or radiation, to make the cancer smaller, so that these treatments are likely to work better.
Is chemotherapy the same as immunotherapy?
No chemotherapy and immunotherapy are not the same. They work in different ways to treat cancer.
- Chemotherapy attacks cells as they divide and can kill both cancerous and healthy cells in the process.
- Immunotherapy works to stimulate your own immune system to recognise and attack cancer cells.
- Examples of immunotherapy are immune checkpoint inhibitors.
Below are some examples of currently funded chemotherapy available in Aotearoa New Zealand.
Chemotherapy available as pills (tablets or capsules)
- capecitabine
- cyclophosphamide
- etoposide
- hydroxycarbamide
- methotrexate
- midostaurin
- temozolomide
- vinorelbine.
Chemotherapy given by injection or infusion
- bendamustine
- carboplatin
- cisplatin
- cyclophosphamide
- dacarbazine
- docetaxel
- doxorubicin
- epirubicin
- etoposide
- fluorouracil (also called 5FU)
- gemcitabine
- irinotecan
- methotrexate
- oxaliplatin
- paclitaxel
- pemetrexed
- vinblastine
- vinorelbine.
Chemotherapy applied to your skin
- fluorouracil cream
- imiquimod cream.
Chemotherapy can travel through your blood and kill cells in your body that grow quickly (eg, cancer cells). It also kills fast-growing normal cells, such as those in your blood, hair and the lining of the gastrointestinal tract. This is why side effects can occur throughout your body.
You can see how chemotherapy works in the video below.
Video: How does cancer chemotherapy work?
(Cancer Centre, US, 2024)
Fortunately, our bodies are good at healing and growing. When normal cells are damaged, they can repair and grow again. Cancer cells lose the ability to manage their growth and to repair themselves, so when they're damaged they're less likely to grow back. This is why chemotherapy can slow or stop the spread of cancer.
The type of treatment that your specialist chooses for you depends on:
- what type of cancer you have
- how far it has spread
- your general health.
Your oncology (cancer specialist) team will keep a close eye on you during your treatment. You may have blood tests, X-rays and scans to see how you're doing. If necessary, your oncology team will change your medicines, the dose or how often they give them to you. Sometimes they will stop the treatment early or recommend you keep taking it for longer than planned. It all depends on how your body and the cancer respond to the treatment.
Chemotherapy can be given in different ways depending on the type of cancer being treated and the medicine used.
It can be given:
- as tablets or capsules that you take by mouth (orally)
- by injection or infusion through a vein (called IV infusion)
- by applying the medicine directly to the area affected by cancer such as a cream you apply to your skin
Sometimes chemotherapy is given by itself, either as tablets or capsules, or in a drip (intravenous or IV infusion). More often, 2 or more medicines are given together.
If many intravenous (IV) chemotherapies are given or blood tests need to be taken often, a central line may be put in to help with these. A central line can be a thin tube inserted into a blood vessel in your arm or chest, or may be a device placed in a large vessel in your chest to allow easy access during your treatments. These lines can be used long term and are often cleaned and checked by nurses.
Chemotherapy doesn't get into your brain, spinal cord or fluid around your brain and spinal cord very well so, for a few cancers, the medicines are inserted into the base of your spine through a process called lumbar puncture.
Is it painful?
Having chemotherapy doesn't usually hurt. If you have a drip (IV) you may feel a brief sting as the needle goes in, but then the pain should stop. However, if you are having an infusion and it feels painful, let a member of the oncology team know immediately.
You may experience side effects after chemotherapy such as pain, nausea and swelling. You will be given medicines and advice on how to manage these. Read more about chemotherapy side effects.
Will I have to stay in hospital?
Most people have their chemotherapy during an appointment as an outpatient. Usually, you have to spend a few hours at the hospital or treatment centre for each treatment. At your treatment, it's likely you will have a blood test first, or on the day before. Your oncology team will check if you're well enough and check the results before they can give you the treatment. Some people may need to stay in hospital overnight or for several days.
If you live a long way from the hospital, you may be able to receive financial support for travel and accommodation. Talk to your treatment team to arrange this. Where possible, you can get support to bring whānau and support people to stay with you.
Driving
You'll probably find it best to get someone to drive you to and from hospital for the first treatment, as you might not feel well enough to drive. If you feel okay to drive after your first treatment, you will probably be fine to do so for following appointments. If you live far away from the hospital, you should arrange for someone to drive you or ask about transport options.
How long will I need chemotherapy?
Your treatment could last several weeks or several months. You will probably get 1 dose of treatment at a time or over a few days, and then you'll be given a rest before having the next treatment. Treatments are usually given in ‘cycles’ which is a period of treatment followed by a rest period. The cycle length varies but generally includes a few days of treatment followed by a few weeks of rest, before starting again.
Spacing out your treatment in this way gives your body a chance to recover from any side effects.
It's important to look after yourself during chemotherapy so that your body is strong enough to cope with the treatments.
- Only do activities you feel comfortable doing. You may find you can mostly go on with your normal life, or you may need to take things much easier.
- Accept help from people who can support you and plan to do as little as possible. Put your needs and wishes first.
- Most people keep working during their chemotherapy and arrange time off to go to hospital for each treatment. Some people work part-time instead of full-time, while others take a few days off around each treatment. Others take an extended break for the whole course of the treatment.
- Talk to your employer, whānau and friends and work out what suits you. There may even be more flexible work arrangements if you make a time to talk about it. Try to not push yourself to do too much.
Blood tests and monitoring
It's likely you'll have regular blood tests before and during each treatment. These may test your blood cell count, liver and renal function and also check markers of your response to chemotherapy. You need to have blood counts because chemotherapy can lower blood cell levels.
If any part of your blood count is too low, your oncology team might give you a longer time between treatments, they may change your chemotherapy or give you another treatment to boost your blood counts.
Taking other medicines
Before you start chemotherapy, give your specialist a list of all the medicines and supplements you're taking, including paracetamol (eg, Panadol), anti-inflammatories (eg, Nurofen), rongoa Māori, vitamins, or treatments from herbalists, naturopaths, homoeopaths or health food stores.
If you want to take any new medicines while having chemotherapy, check with your healthcare provider or specialist about these before you begin taking them. Some chemotherapy doesn't mix well with other medicines or there might be a better time in your treatment to begin them.
There are several support services available, talk to your treatment team for further recommendations.
How can we help?(external link) Cancer Society of NZ, 2022
Emotions and cancer(external link) Cancer Society of NZ, 2022
Questions you may wish to ask [PDF, 498 KB] Cancer Society of NZ, 2022
Questions to ask your doctor about chemotherapy(external link) Cancer Society of NZ, 2022
Find a cancer hospital/service near you(external link) Healthpoint, NZ
Cancer(external link) Te Aho o Te Kahu – Cancer Control Agency
National Travel Assistance Scheme(external link) Health New Zealand | Te Whatu Ora
Cancer support Healthify
Patient Information sheets(external link) eviQ, Australia
Chemotherapy(external link), immunotherapy(external link), targeted treatment(external link) Cancer Society, NZ
Living well with cancer – eating well [PDF, 5.5 MB] Cancer Society, NZ English/te reo Maori [PDF, 5.5 MB]
Brochures
Medicines and side effects [PDF, 91 KB](external link) Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
Living well with cancer – eating well Cancer Society, NZ English/te reo Māori
References
- Chemotherapy(external link) American Cancer Society
Brochures
Chemotherapy, Immunotherapy and Targeted Treatment
Cancer Society, NZ, 2019
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
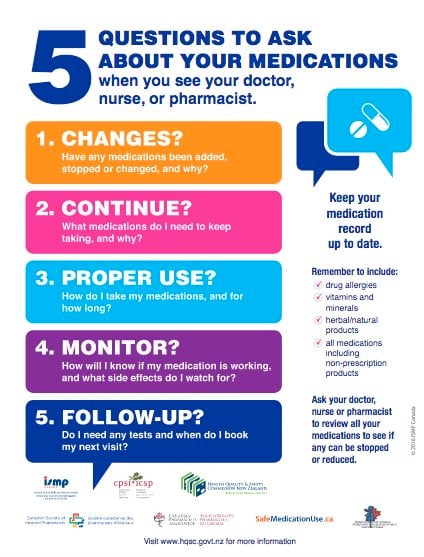
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Healthify clinical advisors
Last reviewed:





