If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Snoring or noisy breathing in children
Also known as obstructive sleep apnoea in children
Key points about snoring or noisy breathing in children
- Snoring or noisy breathing during sleep may be a sign that your child is having difficulty breathing and may have obstructive sleep apnoea (OSA).
- OSA is a medical condition where narrowed breathing passages make breathing more difficult during sleep.
- Snoring can have long-term effects on sleep quality, behaviour and learning.
- Enlarged tonsils and adenoids are an important cause of OSA, and an operation to remove them can fix the problem.
- Overweight tamariki are at greater risk of OSA.
- See your healthcare provider if your child often snores or has noisy breathing.
- The content on this page comes from KidsHealth(external link).

It's normal for tamariki to sometimes make noises with breathing during sleep. It's not normal for tamariki to snore unless they are unwell with a cold.
Noisy breathing can come from the nose or from an open mouth. It can be worse when your child is sleeping on their back. If you notice snoring or noisy breathing often during your child's sleep, talk to your healthcare provider. It might be a sign of a condition called obstructive sleep apnoea (OSA).
Narrowed breathing passages make breathing more difficult during sleep
When someone falls asleep, the muscles of the throat relax and the breathing passages at the back of the nose and in the throat become narrower. In tamariki, the tonsils and adenoids can grow to be quite large, and less air gets through the breathing passages during sleep. When this happens, you may notice snoring or noisy breathing.
Snoring is more common during some phases of sleep
There are some times during sleep when the muscles are more relaxed. Snoring is more common during these phases of sleep. This is why snoring can be more common in the second half of the night.
Snoring needs checking
Snoring is not always a very serious problem for tamariki – about 15 to 20% of tamariki snore. But, it is a symptom that needs checking by your healthcare provider as 2 to 5% of tamariki have OSA.
Reasons for OSA
In tamariki, the most common reason for OSA is enlarged tonsils and adenoids. In older tamariki and rangatahi (young people), being overweight is a common reason. Any medical condition that affects the size and shape of your child's breathing passages can also make OSA more likely.
The image below shows an open mouth with enlarged tonsils.
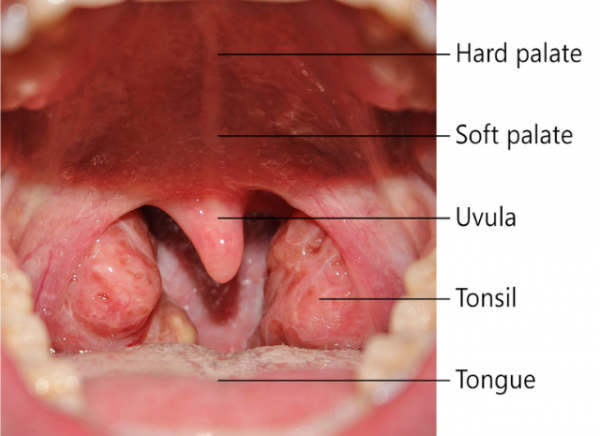 Image credit: Klem via Wikimedia Commons(external link)
Image credit: Klem via Wikimedia Commons(external link)
In OSA, the narrowing of the breathing passages at the back of the nose and in the throat during sleep is enough to cause breathing difficulty or pauses in breathing. A child wakes up briefly because they cannot breathe properly, often with a loud gasp or snort. These episodes can happen many times through the night. The disturbed sleep can result in changes in behaviour during the day such as:
- poor attention and lack of concentration
- hyperactive behaviour
- seeming 'fragile' or 'oversensitive' or 'overtired' or 'grumpy'
- being impulsive (tending to act without thinking)
- difficulty learning at school because of issues with concentration
- sleepiness – but this is more common in rangatahi and adults than tamariki.
Severe OSA can cause high blood pressure and put strain on the heart. This is not as common in tamariki as in adults but it is something your healthcare provider will look for.
Signs of possible OSA in a child who snores include:
- restlessness during sleep (moving around the bed a lot)
- short pauses in breathing – their chest is moving but no air is moving through their nose and mouth
- needing to make more effort to breathe
- sweating during sleep
- mouth breathing when asleep or awake – the passage to their nose may be completely blocked
- daytime behaviour issues (see the section above).
Video: Noisy breathing in a child with obstructive sleep apnoea
This video shows a child with severe OSA. You can see his chest sucking in with each breath. The noises you can hear are because his breathing passages are partly blocked.
If you're worried that your child may have OSA, take them to your healthcare provider. They will examine your tamariki and may recommend they see:
- an ear, nose and throat surgeon if your healthcare provider thinks the tonsils and adenoids are causing the problem, or
- a paediatrician (a doctor who treats children).
Your healthcare provider will want to know all about your child's sleep patterns. They will examine your child's breathing passages by looking into their mouth and nose. It can be very helpful for you take a video (on your phone) of your child sleeping. Try to film the breathing pattern you're most concerned about so that you can show this to your healthcare provider.
Your child may not need any further investigations if it's clear your child has OSA.
For some tamariki, your healthcare provider may recommend your child has an overnight oximetry test or a sleep test (polysomnography).
Read more about oximetry(external link) and polysomnography.(external link)
The treatment for OSA depends on its cause. The most common treatment is removing the tonsils or adenoids (or both tonsils and adenoids) to open up the breathing passages.
Tamariki who have this surgery need to go back to their healthcare provider 6 to 8 weeks after their surgery. The healthcare provider will check that their symptoms are better.
Read more about tonsillectomy and adenotonsillectomy.(external link)
Removing tonsils or adenoids (or both) can fix OSA. Some tamariki keep having symptoms after surgery. This is more common in overweight tamariki.
If surgery isn't recommended for your child, or if your child keeps having symptoms after removal of their tonsils or adenoids (or both), they may need further tests. They might need an overnight oximetry test(external link) or a sleep test (polysomnography)(external link).
Some tamariki will need further treatment, which may include:
- a weight management programme
- treatment to help with breathing during sleep, eg, CPAP (continuous positive airway pressure)(external link)
- more surgery.
Snoring and sleep apnoea in children (PDF, 13KB)(external link) Sleep Disorders Australia
Obstructive sleep apnea(external link) KidsHealth, Nemours Foundation, US
Credits: This content has been collaboratively developed by Health New Zealand | Te Whatu Ora, KidsHealth, and Healthify He Puna Waiora to provide trusted health information.
Last reviewed:





