Skin cancer prevention and early detection strategy 2024 – 2028(external link) Melanoma Network, NZ, 2025
Reducing the burden of melanoma in NZ part 1 – prevention and risk assessment(external link) BPAC NZ, January 2020
Reducing the burden of melanoma in NZ part 2 – early detection of melanoma(external link) BPAC NZ, January 2020
Topical treatments for non-melanoma skin cancers
The Best Practice team provides a useful summary of how fluorouracil and imiquimod creams can be used as topical treatments for non-melanoma skin cancers:
- Fluorouracil and imiquimod creams are topical treatments that may be used to treat some non-melanoma skin cancers, usually second-line to surgical excision and/or cryotherapy.
- Special Authority approval is no longer required for subsidy.
- These medicines work by destroying cancerous cells in the skin, resulting in a local reaction including erythema and erosion, followed by re-epithelisation of the skin.
- Fluorouracil and imiquimod may be appropriate for the treatment of actinic keratoses, superficial basal cell carcinoma and squamous cell carcinoma in situ.
- Treatment regimens vary depending on the type of lesion, but fluorouracil and imiquimod creams are typically applied daily or several times a week, for four to 12 weeks or longer.
See full guidance: How to use fluorouracil and imiquimod for non-melanoma skin cancer in a general practice setting(external link) BPAC, NZ, 2017
Skin lesion management guidelines
The following advice is taken from Managing non-melanoma skin cancer in primary care – a focus on topical treatment(external link) BPAC, NZ, 2013
If a patient presents with a suspicious lesion:
- Assess the likelihood of melanoma being present then provisionally identify the type of lesion.
- Surgical excision with histology is the first-line treatment for all skin cancer. It has the highest cure rate among available treatments.
- Referral, according to local guidelines, to a General Practitioner with a Special Interest (GPSI) in skin lesions, a Dermatologist, a Plastic Surgeon or an ENT Surgeon may be appropriate for patients with large lesions or lesions with an aggressive growth pattern.
- Patients with superficial basal cell carcinoma or intraepidermal carcinoma (squamous cell carcinoma in situ) may be safely managed with cryotherapy or topical treatments, i.e. fluorouracil or imiquimod creams, when excision is not appropriate because of the location of the lesion or due to cosmetic considerations.
- Topical treatments should not be considered if the diagnosis is uncertain.
Red-flags: Is this melanoma?
Look for features of a melanoma using the ABCDE rule or the seven-point checklist.
|
|
The ABCDE rule |
|---|---|
|
A |
Asymmetry |
|
B |
Border irregularity. |
|
C |
Colour variation. Note: Black is not essential and may not be present in some melanomas, ie, nodular or amelanotic melanoma. |
|
D |
Diameter > 6 mm. However, melanoma can be diagnosed when less than this diameter. |
|
E |
Evolution and/or elevation, eg, lesions may enlarge and a flat lesion may become raised in a matter of a few weeks. |
|
Seven-point checklist |
|
|---|---|
|
Major features: |
|
|
1 |
Change in size of previous lesion or obvious growth of a new lesion |
|
2 |
Irregular shape |
|
3 |
Irregular colour with a variety of shades of brown and black |
|
Minor features: |
|
|
4 |
Diameter > 6 mm |
|
5 |
Inflammation |
|
6 |
Oozing, crusting or bleeding |
|
7 |
Change in sensation |
To help with identification DermNet NZ for images of:
- melanoma(external link)
- actinic keratosis(external link)
- basal cell carcinoma (BCC)(external link)
- cutaneous horn(external link) (acutaneous horn can be based on viral warts, actinic keratosis or squamous cell carcinoma)
- squamous cell carcinoma (SCC)(external link)
- SCC in situ(external link).
Prevention and early detection strategy
The NZ skin cancer primary prevention and early detection strategy 2017 to 2022(external link) identifies 5 intervention pathways for reducing incidence, impact and inequalities with respect to skin cancer:
- primary prevention
- early detection
- diagnosis and treatment
- rehabilitation, support and palliative care
- research, evaluation and surveillance.
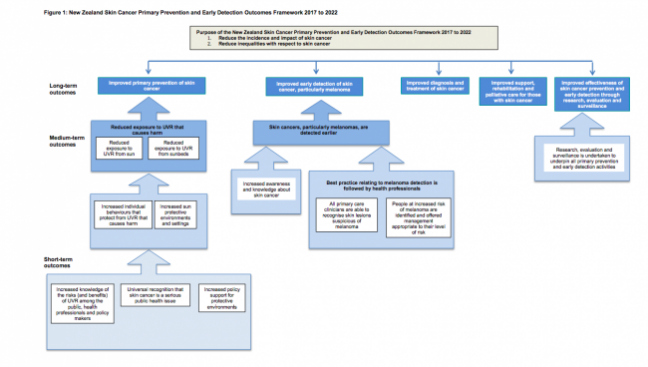
Image: Health Promotion Agency
Melanoma risk calculator(external link) Best Practice, NZ



