Prostate cancer | Mate pukupuku repe tātea
Key points about prostate cancer
- Prostate cancer (mate pukupuku repe tātea) is the most common type of cancer for New Zealand men.
- It's most common in men over 50 years of age, but can occasionally occur in those who are younger.
- If caught early, prostate cancer can be managed well and can usually be cured, but not all prostate cancer needs to be treated.
- In particular, if you’re 50+ years of age, tell your healthcare provider if you have any lower urinary tract symptoms such as poor flow of urine (pee), trouble starting or stopping urinating, needing to urinate more often and urgently, or incontinence (leaking urine).

The prostate gland is only found in men. It's a small walnut-shaped gland that surrounds the opening of your bladder. It helps make semen.
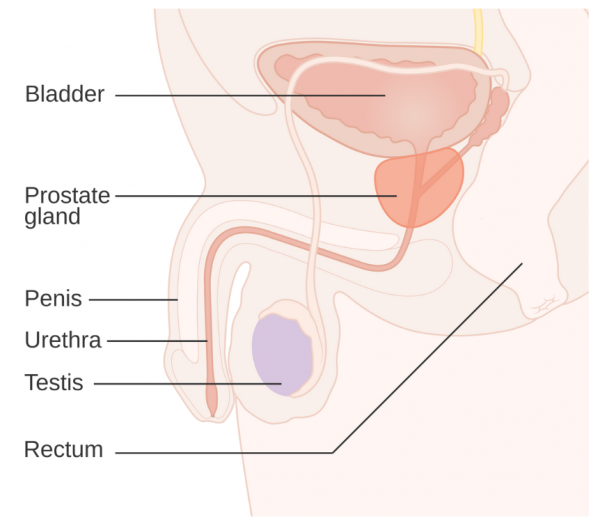
Image credit: CRUK via Wikimedia Commons(external link)
As men get older, the prostate gland increases in size and can cause prostate enlargement, known as benign prostatic hyperplasia or BPH. From 50 years of age, men often experience problems with urination (peeing) due to this. This is much more common than prostate cancer.
Prostate cancer is caused when some of the cells within your prostate gland start to grow out of control, invading and destroying healthy cells. Most commonly, prostate cancer grows slowly, but sometimes it can grow rapidly and spread to other areas, such as your bones, liver and lungs. This is known as metastatic cancer.
In Aotearoa New Zealand, more than 4,000 men are diagnosed with prostate cancer every year and 650 die from the condition. Prostate cancer is the most common cancer in New Zealand men and the third most common cause of cancer death in men.
The number of men diagnosed with prostate cancer in Aotearoa New Zealand has been increasing but the rate of newly diagnosed cancer and the rate of people dying from prostate cancer has been slightly decreasing. The rate refers to the number of individuals per population. Over time, more people have been tested and successfully treated for prostate cancer.
Māori men are slightly less likely than non-Māori men to develop prostate cancer, but if they do develop the condition, they're then more likely to die of it because it's more often found too late to cure.
Early prostate cancer causes no symptoms. As the cancer grows, it can cause urinary symptoms, eg, problems with flow or irritation of your bladder. These include:
- poor flow of urine
- trouble stopping
- dribbling after you have finished urinating (peeing)
- needing to urinate more often, at night or urgently
- trouble starting to urinate
- incontinence (not being able to control when you urinate)
- pain when urinating
- blood in your urine.
Most of the time these symptoms are due to other common problems such as benign enlargement of the prostate gland or urinary tract infection (UTI). However, if you have any of these symptoms let your healthcare provider know so they can assess your risk of getting prostate cancer and provide advice on whether or not to do prostate testing.
In the late stage of prostate cancer, the cancer cells might spread to other parts of your body and cause symptoms such as:
- new bone or back pain
- both legs swelling
- numbness or weakness in both legs
- nausea or vomiting
- breathlessness
- visible blood in your urine
- inability to urinate
- loss of appetite
- weight loss
- fatigue or extreme tiredness.
| These symptoms and signs are not normal, but may also be due to other non-cancer related conditions. If you have any of these symptoms see your healthcare provider quickly. |
- Age – the risk of prostate cancer increases as you age. It is generally rare in men under the age of 50, but after that the risk increases. Much older men who get prostate cancer may not need treatment as other co-existing medical conditions may be more important to manage.
- Family history – you have double the chance of getting prostate cancer if your father or brother has had prostate cancer. If several close relatives have (or have had) prostate cancer, and this is at a younger age, your relative risk may be even higher.
- Genetics – your risk of prostate cancer is higher if you have the BRCA 1 or 2 gene. Read more about the BRCA gene.
- Abnormal prostate testing – if you have done a PSA blood test and a digital rectal examination before and been told that the results are abnormal, have this assessed for prostate cancer.
- Other factors – there is less clear evidence, but other factors may include exposure to certain chemicals or diet. Having been a smoker doesn't appear to increase risk but of you do have prostate cancer and you smoke, the outcome is likely to be worse.
Routine testing for prostate cancer (eg, for people without urinary symptoms and without the obvious risk factors listed above) isn't recommended. This is because the tests we have are not all that accurate enough. The tests may suggest cancer which is not actually there or they may miss cancer that is there. This may cause unnecessary anxiety or provide false reassurance.
If you're not sure if you need to get tested for prostate cancer, discuss the risks and benefits of testing with your healthcare provider. Having a prostate check is your decision, based on your circumstances including the risk factors listed above.
Checks usually involve a blood test called a prostate-specific antigen (PSA) test and a digital rectal examination (DRE). Read more about prostate cancer testing.
If you have an abnormal PSA test and abnormal digital rectal examination, further tests, such as an MRI scan and a prostate biopsy, are needed to diagnose prostate cancer and confirm the presence of cancer cells.
Video: MRI for prostate diagnosis
The video below describes how a different scan (PSMA PET CT scan) can be used to see where the cancer is and how far it's spread. It's available in private health care only.
Video: Prostate cancer diagnosis and treatment
If you have prostate cancer, you will be referred to a specialist (urologist) and then possibly a radiation oncology specialist. The choice of treatment depends on the size, type, growth and spread of the cancer, and your age, general health, symptoms and ultimately your informed, personal choice.
Treatment options for prostate cancer include active surveillance, surgery, radiation therapy (radiotherapy), hormone therapy and palliative care.
Most people want to know whether their cancer can be successfully treated. The outcome of the treatment will depend on the type of cancer and whether it has spread, how quickly it grows, and how well the treatment works. If the prostate cancer is localised to the prostate gland, it's sometimes slow growing and may never need treatment. Other localised prostate cancers do require treatment and often it's possible to successfully get rid of the cancer. If the cancer has spread outside of the prostate gland, treatments can often keep it under control for many years.
Prostate cancer classification
Prostate cancer is classified by the Gleason Score. A Prostate Cancer Gleason Score helps to determine how aggressively the prostate cancer is likely to behave and how quickly it's likely to grow. The score is also an indicator of how likely it is to spread beyond the prostate gland. The Prostate Cancer Gleason Score score ranges from 2 to 10. To determine the Gleason score, the pathologist uses a microscope to look at the patterns of cells in the prostate tissue. The cell pattern is given a grade of 1 (most like normal cells) to 5 (most abnormal). If there is a second most common cell pattern, the pathologist gives that pattern a grade of 1 to 5 as well. The pathologist adds the 2 most common grades together to make the Gleason score. If only 1 pattern is seen, the score for that pattern is used twice (eg, 5 + 5 = 10). A high Gleason score (such as 10) means a high-grade prostate tumour. High-grade tumours are more likely than low-grade tumours to grow quickly and spread.
The International Society of Urological Pathology (ISUP) grading system uses the Gleason score to further grade the cancer. The lower the grade the less likely the cancer is going to spread. The grade helps your specialist to plan your treatment:
- Grade group 1: Gleason score 6 or lower (low-grade cancer)
- Grade group 2: Gleason score 3 + 4 = 7 (medium-grade cancer)
- Grade group 3: Gleason score 4 + 3 = 7 (medium-grade cancer)
- Grade group 4: Gleason score 8 (high-grade cancer)
- Grade group 5: Gleason score 9 to 10 (high-grade cancer)
Prostate cancer management
Management options for prostate cancer include active surveillance (watch closely and regularly), or treatment such as surgery, radiation therapy (radiotherapy), hormone therapy or chemotherapy.
Active surveillance (no active treatment, but watch and wait)
No treatment is provided and instead, you are monitored regularly with blood tests or other investigations (eg, scans and biopsies), either in hospital or by healthcare provider follow-ups. This option is usually recommended if you have an early stage of prostate cancer or your cancer is slow growing. This is because it may not be of benefit to have treatment if the cancer isn't affecting your quality of life – and it may never do so. Active surveillance can also be offered if you have a late stage of prostate cancer and the management of other health conditions is more important.
Surgery
This can be an option if it's possible to remove all the cancer cells by taking out part or all your prostate. The aim of surgery is to cure your prostate cancer. As with any type of surgery there are risks. With prostate cancer surgery risks include bleeding, infection, scar formations (stricture), incontinence (unable to control urine) or impotence (unable to get or maintain an erection)
Radiation therapy (radiotherapy)
The aim of radiotherapy is also to cure your prostate cancer. Radiotherapy has side effects such as pain when peeing, loose bowel motions, bleeding from your rectum, impotence and more. Your healthcare team will explain more to you when discussing treatment options. Read more about radiotherapy.
Hormone therapy
Testosterone helps prostate cancer cells grow. Hormone therapy involves giving you medicines to stop your testicles from producing the male hormone testosterone. These medicines are called luteinizing hormone-releasing hormone (LHRH) analogues (eg, goserelin). Another name for these medicines is gonadotropin-releasing hormone anologs. Other medicines that stop testosterone from acting on cancer cells are known as anti-androgens (eg, bicalutamide, cyproterone) and they're often used together with LHRH analogues.
Palliative care
This is usually offered to people with later-stage or advanced cancer. Treatment is focused on relieving your symptoms. Read more about palliative care.
The video below, talks about fatigue associated with prostate cancer and how you can manage it.
Video: What is fatigue? | Prostate Cancer UK
Fatigue is extreme tiredness. 3 in 4 men with prostate cancer will experience it at some point.
You can reduce your risk of prostate cancer by finding the cancer early and by having a healthy lifestyle.
Healthy lifestyle choices include:
- having a low-fat, high-fibre diet that includes plenty of fresh fruits and vegetables
- maintaining a healthy body weight
- exercising regularly
- getting enough vitamin D
- being smokefree will be good for your overall health even if it doesn't increase your risk of developing prostate cancer.
Below are some support services and information for people affected by cancer and their family/whānau:
Emotions and cancer English/te reo Māori(external link) Cancer Society, NZ
How we can help(external link) Cancer Society, NZ
Cancer services – find a hospital/service near you(external link) Healthpoint, NZ
Support groups nationwide(external link) Prostate Cancer Foundation, NZ
Video: 10 years with prostate cancer | Rob and Robyn McFarlane
Rob and Robyn McFarlane share their personal journey with Prostate Cancer Foundation Ambassador Jason Gunn.
(Prostate Cancer Foundation of NZ, 2020)
Video: Coping with fatigue after cancer treatment – Denton's story
Denton describes how he coped with fatigue (tiredness) during his treatment for prostate cancer. He talks about the physical and emotional effects, feeling unable to do anything and being isolated. Denton tells us how he found ways to cope.
The following links provide further information about prostate cancer. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Is a check right for you?(external link) Kupe, NZ
Prostate cancer(external link) Te Aho o Te Kahu – Cancer Control Agency, NZ
Prostate cancer testing(external link) Better Health Channel, Australia
Resources
Low risk prostate cancer – don't rush to get treatment(external link) Choosing Wisely, NZ
Prostate cancer – Understanding Cancer: A guide for men with prostate cancer(external link) Cancer Society of New Zealand Inc
References
- Prostate cancer(external link) Cancer Control Agency Te Aho O Te Kahu, NZ, 2024
- Prostate cancer diagnosis(external link) Canterbury Regional HealthPathways, NZ, 2023
- Prostate cancer established(external link) Canterbury Regional HealthPathways, NZ, 2022
- Prostate cancer testing decision support tool for patients and their families(external link) BPAC, NZ, 2018
- Gleason grading system(external link) Medline, US, 2024
- The prostate(external link) Prostate Cancer Foundation, NZ, 2024
See our page Men's health for healthcare providers
Brochures
Choosing Wisely, NZ, 2018

Prostate cancer – understanding cancer: A guide for men with prostate cancer
Cancer Society of New Zealand Inc, 2019
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Roland Meyer, Specialist Physician, Respiratory and General Medicine
Last reviewed:





