Hiccups in palliative care
Key points about hiccups and palliative care
- Hiccups are caused by an uncontrollable contraction of your diaphragm.
- Your diaphragm is the muscle that separates your abdomen from your chest. The contraction causes your vocal cords to close briefly, resulting in the hiccup sound.
- Hiccups can be very distressing.
- There are many causes that can contribute to hiccups if you have a terminal illness.

Hiccups are caused by an uncontrollable contraction of your diaphragm, the muscle that separates your abdomen (stomach) from your chest. The contraction causes your vocal cords to close briefly, resulting in the hiccup sound.
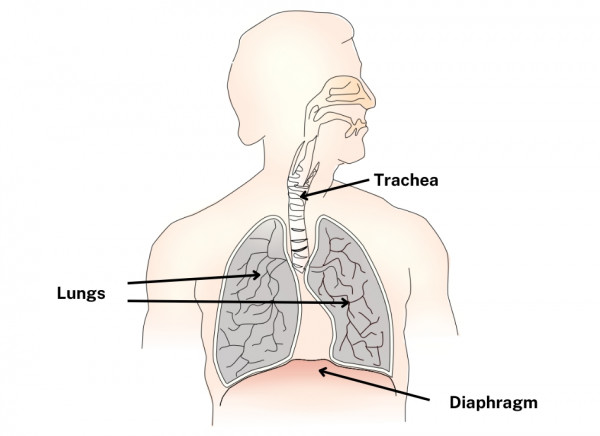
Image credit: Openclipart via Wikimedia Commons
The repeated contraction or spasm of your diaphragm can happen for a short time, or can continue for days or longer. Having hiccups that last longer than 48 hours isn’t uncommon for people with advanced cancer and can be very upsetting.
There are many possible causes of hiccups. Common causes of hiccups for people living with a life-limiting illness include:
- Gut problems, such as stomach distension or gastroparesis (when your stomach takes a long time to empty) – these are the most likely cause
- gastro-oesophageal reflux (GORD)
- conditions affecting your metabolism
- liver disease
- conditions affecting your brain, such as stroke, brain tumour, head injury or brain infection
- Irritation of the nerves that supply your diaphragm, such as the phrenic nerve and the vagus nerve, due to surgery, tumours or infections.
Talk to your healthcare team about your hiccups. They may ask you some questions to find out the possible causes of your hiccups. They may also examine you.
Some tests may also be done, depending on what your doctor thinks is causing your hiccups. These include:
- blood tests such as full blood count, kidney function tests or liver function tests
- imaging tests such as ECG, chest X-ray or CT scan.
If you have a medical condition, or any obvious cause for your hiccups, treatment will focus on the condition or cause.
Otherwise, treatment of hiccups can include things you can try yourself, or treatment with medicines.
Things to try for hiccups
If you know what gives you the hiccups, such as eating too much or eating or drinking specific things, try to avoid those to see if it helps.
If not, there are a number of things you can try to see if they stop your hiccups – some may work, some not but they’re worth trying. You may need somebody to help you with some of them.
- Hold your breath for a short time.
- Take deep breaths.
- Breathe into a paper bag (not plastic).
- Suck on a lemon (rinse your mouth with water afterwards as the acid can affect your teeth).
- Eat a small slice of fresh ginger.
- Drink a glass of water slowly.
- Drink from the wrong side of a glass.
- Suck on an ice cube or eat ice chips.
- Gargle with water
- Get someone to scare you.
- Have someone pull on your tongue.
- Bend from the waist or sit down and lean forward over your knees to compress your diaphragm.
- Reach up and hang from a door frame. By stretching out your diaphragm, it might ease the spasms.
- Use a swab to rub your soft palate.
Medicines
There's a range of medicines that may help with your hiccups, depending on the cause. Your healthcare provider can talk to you about medicines that may help by relaxing your muscles, reducing stomach bloating, or controlling the hiccup reflex.
- metoclopramide
- chlorpromazine
- baclofen
- dexamethasone
- gabapentin
- haloperidol
- midazolam
- nifedipine
- simeticone.
Sometimes, hiccups can be difficult to manage despite having treatment.
The following links provide further information about hiccups. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Managing the symptoms of cancer(external link) Macmillan Cancer Support, UK
Hiccups(external link) NHS, UK
Hiccups(external link) Patient Info, UK
References
- Hiccups in palliative care(external link) Auckland Regional HealthPathways, NZ, 2020
- Managing the symptoms of cancer(external link) Macmillan Cancer Support, UK
- Hiccups, dyspepsia and reflux in palliative care(external link) Marie Curie, UK, 2022
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Tom Middlemiss, Palliative Care Specialist, Te Omanga Hospice
Last reviewed:





