The content on this page covers medicines for short-term pain. For information about medicines for pain that continues for 3 months or longer, see pain relief medicines for chronic pain. Read more about the difference between acute pain and chronic pain.
What is short-term pain?
Short-term pain is also commonly called acute pain. Acute pain usually occurs because of surgery, injury or infection, such as a dental infection or bone fracture (break). It often comes on quickly, lasts for a short time and goes away as the underlying cause gets better. Pain relieving treatments usually only need to be given for a short time while the injury is healing.
- Paracetamol and NSAIDs are commonly used.
- Opioids are useful and usually only need to be given for a few days. The dose of opioid should be reduced as healing occurs.
- Read more about acute pain.
Severity of the pain
Pain is usually grouped into mild pain, moderate pain or severe pain. The step-wise or ladder approach to managing pain is based on the severity of your pain. It's a 3-step approach.
- Step 1: Mild-to-moderate pain – this type of pain is best treated with paracetamol, ibuprofen and other NSAIDs. Read more about paracetamol and NSAIDs.
- Step 2: Moderate-to-severe pain – more intense pain is treated with mild opioid pain relievers such as codeine and tramadol. These may be used together with paracetamol or NSAIDs.
- Step 3: Severe pain – severe pain is treated with strong opioids such as morphine and oxycodone. These may be used together with paracetamol or NSAIDs. Read more about opioids.
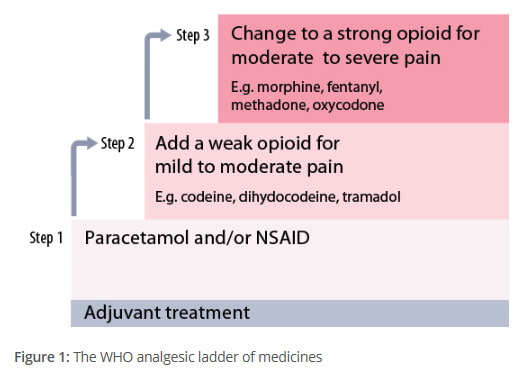
Image credit: The principles of managing acute pain in primary care(external link), BPAC