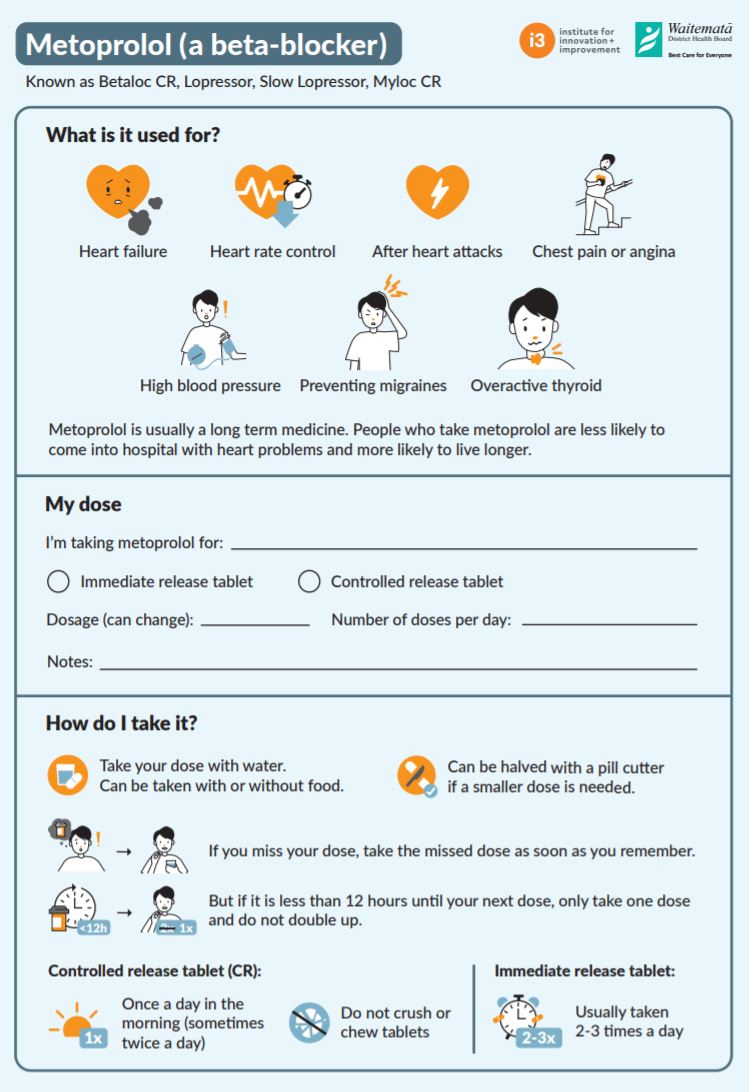
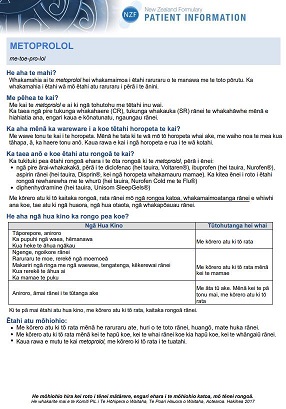
Metoprolol is used to treat many conditions including heart failure, high blood pressure (hypertension), and irregular heart beat. It may also be prescribed after a heart attack (to prevent heart damage). Metoprolol is also used to prevent migraine headaches.
It belongs to a group of medicines called beta-blockers. Metoprolol works by slowing down your heart rate and making it easier for your heart to pump blood around your body.