You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Upadacitinib
Say 'ue-PAD-a-SYE-ti-nib'
Key points about upadacitinib
- Upadacitinib is used to treat inflammatory conditions such as rheumatoid arthritis, Crohn's disease, ulcerative colitis and atopic dermatitis (eczema).
- Upadacitinib is also called Rinvoq.
- Find out how to take it safely and possible side effects.

Upadacitinib is used to treat inflammatory conditions such as rheumatoid arthritis, Crohn's disease, ulcerative colitis and atopic dermatitis (eczema). Upadacitinib belongs to a group of medicines called janus kinase (JAK) inhibitors. It works by blocking a substance in your body called janus kinase, thought to cause inflammation. Upadacitinib is an immunosuppressive medicine, which helps to calm an overactive immune response.
In Aotearoa New Zealand upadacitinib is funded under a Special Authority for people who meet certain criteria. A special authority means your specialist will need to make an application to Pharmac (the government medicine funding agency) for approval before the medicine can be funded for you.
Rheumatoid arthritis
- Upadacitinib helps to reduce joint pain, swelling and stiffness and slows or stops further joint damage.
- It's prescribed when commonly used medicines such as methotrexate and other less commonly used medicines like biologics don't work well enough or are unsuitable. Read more about rheumatoid arthritis.
Crohn’s disease and ulcerative colitis
- Upadacitinib helps to reduce diarrhoea, an urgent need to go for a poo, abdominal (tummy) pain, bleeding from your bottom and fatigue. It helps to reduce the impact of these symptoms on your quality of life.
- It’s prescribed when biologics don't work well enough or are unsuitable. Read more about Crohn’s disease and ulcerative colitis.
Atopic dermatitis (eczema)
- Upadacitinib helps to reduce itching and flares. It helps to improve the condition of your skin and the impact of eczema on your quality of life, such as sleep disturbance.
- It’s prescribed for moderate to severe eczema, when immunosuppressive medicines (such as azathioprine, ciclosporin, methotrexate or mycophenolate mofetil) and topical steroids or calcineurin inhibitors (pimecrolimus, tacrolimus) have not worked well or are unsuitable. Read more about atopic dermatitis.
- Note: It‘s important to continue using emollients and topical steroids while you're taking upadacitinib to manage your eczema. Studies have shown that combining upadacitinib with topical steroids during flare-ups can lead to better results.
In Aotearoa New Zealand upadacitinib is available as tablets (15 mg, 30 mg and 45 mg).
- Always take upadacitinib exactly as your healthcare provider has told you. The pharmacy label on your medicine will tell you how much to take, how often to take it and any special instructions.
- The dose of upadacitinib will be different for different people depending on what it’s being used for.
- Timing: Take upadacitinib tablets once a day. You can take it with or without food. Take your tablet about the same time each day.
- Swallow your tablet whole with a glass of water: Do not crush, chew or break the tablets.
- Missed dose: If you forget to take your dose, take it as soon as you remember. But if it's nearly time for your next dose, just take the next dose at the right time. Do not take double the dose.
- Keep taking upadacitinib regularly: Upadacitinib is an ongoing treatment. You may notice an improvement in your symptoms within the first few weeks of treatment, though it can take up to 3 months to improve. Don't stop taking upadacitinib without talking to your healthcare provider first. Your healthcare provider may recommend a break from treatment if you have side effects. Follow their advice for this so you know what to do, and how to re-start treatment.
Here are some things to know when you're taking upadacitinib. Other things may be important as well, so ask your healthcare provider what you should know about.
Tests and monitoring
While you're taking upadacitinib, you'll need regular blood tests to monitor for side effects and to check whether the treatment is working. Blood tests are very important during the first few months of treatment. Over time, these tests are needed less often.
Increased risk of infections
Upadacitinib weakens your body’s defence (immune) system, which means you may be more likely to get infections. Try to avoid close contact with anyone who has chickenpox or shingles. Tell your healthcare provider straight away if you develop symptoms of shingles (a painful rash with blisters) or signs of an infection, so you can be treated straight away.
Vaccines
Vaccines are important because upadacitinib lowers your immune response and increases the risk of infections. Vaccines help reduce the risk of serious infections while on upadacitinib.
- Always tell your healthcare provider that you're taking upadacitinib before having any vaccines.
- Inactivated (non-live) vaccines are safe, such as the annual flu vaccine and COVID-19 vaccines. Keep up to date with these vaccines to reduce your risk of these infections.
- Protection against shingles is important. Ask your healthcare provider about the Shingrix vaccine, which is safe to use. Read more about Shingrix vaccine.
- It's important to avoid live vaccines while taking upadacitinib such as measles, mumps and rubella (MMR) vaccine. If a live vaccine is needed, it’s usually given before starting upadacitinib, not during treatment. Read more about live vaccines.
- If you’re a woman under 45 and you don’t have immunity to rubella, doctors are advising you to get the MMR vaccine.
Taking other medicines
Upadacitinib interacts with some medicines, herbal supplements and rongoā Māori, so check with your healthcare provider or pharmacist before starting upadacitinib and before starting any new products.
If you're pregnant, planning a pregnancy or breastfeeding
You should not become pregnant while you're taking upadacitinib and for 4 weeks after stopping treatment. Discuss with your healthcare provider which types of contraception are suitable for you and your partner. If you and your partner are planning a pregnancy, talk to your healthcare provider about other suitable medicines. Do not breastfeed if you're taking upadacitinib.
Like all medicines, upadacitinib can cause side effects, although not everyone gets them. If you're concerned about any symptoms, talk to your healthcare provider. The following information offers some guidance but doesn't include all possible side effects.
Common side effects
Tell your healthcare provider if these side effects bother you.
- Indigestion, tummy upset.
- Headache.
- Fatigue (feeling unusually tired and weak).
- Weight gain.
- Acne.
Tell your healthcare provider immediately or phone Healthline free on 0800 611 116 if these occur
- Signs of blood clots, such as swelling or pain and tenderness in your leg, sudden chest pain and shortness of breath.
- Signs of infection in your lung (pneumonia), such as shortness of breath, fever and a cough with mucus.
- Signs of TB such as a cough that won’t go away, night sweats, fever or weight loss.
Phone 111 for an ambulance or go to your nearest accident and emergency (A&E) clinic if these occur
- Signs of an allergic reaction such as muscle or joint pain, fever, rash, intense itching, swelling of the face or hands, sore throat, headache, or difficulty swallowing.
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
Rinvoq(external link) Medsafe Consumer Information Sheet, NZ
Upadacitinib(external link) Arthritis Australia
Upadacitinib(external link) British Association of Dermatology
Upadacitinib(external link) Crohn's and Colitis UK
Brochures
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
Medicines and side effects [PDF, 91 KB] Healthify He Puna Waiora, NZ, 2024
References
- Rinvoq(external link) Medsafe, NZ
Brochures
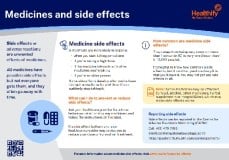
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





