If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Betamethasone cream, ointment and lotion
Key points about betamethasone cream, ointment and lotion
- Betamethasone cream, ointment and lotion are used to reduce inflammation and itchiness from skin conditions such as eczema or dermatitis and psoriasis.
- It’s also called Beta®, Betnovate® and Diprosone®.
- There are different strengths and brands available in Aotearoa New Zealand.
- Find out how to apply them safely and possible side effects.

Betamethasone cream, ointment and lotion are used to reduce inflammation and itchiness from skin conditions such as eczema, dermatitis or psoriasis. They work by reducing the inflammation which can help to ease symptoms such as itchiness and redness. Betamethasone belongs to a group of medicines known as topical steroids.
There are different betamethasone preparations available in Aotearoa New Zealand. They have different uses depending on their strength.
Potent betamethasone preparations
- Betamethasone dipropionate 0.05% (Diprosone® cream or ointment).
- Betamethasone valerate 0.1% (Beta® cream or ointment, Betnovate® lotion, Beta® Scalp application).
Very potent betamethasone preparations
Betamethasone dipropionate 0.05% (Diprosone OV®) is a stronger preparation that's only available as an ointment. The steroid is in an optimised vehicle (OV) of white soft paraffin, beeswax and propylene glycol.
Both potent and very potent betamethasone preparations are usually used to treat moderate to severe skin conditions such as eczema or psoriasis on the body, hands, arms or legs which have a lot of inflammation (redness) and/or thickened skin.
The correct one to use depends on your symptoms, where it is on your body and any irritation (stinging) or allergy.
- Creams are usually best for treating moist areas of skin, and they absorb into the skin well.
- Ointments tend to be greasy and are usually best for treating areas of skin that are dry or thickened. They have the lowest chance of burning and stinging when applied.
- Lotions are easy to apply and may be useful to treat hairy areas such as your scalp.
Use topical steroids as advised by your healthcare provider. They will explain where, how often and for how long to apply the medicine.
- Creams or ointments are rubbed gently into the affected skin until they have disappeared.
- The amount of topical steroid you should apply is measured in fingertip units (FTUs). One FTU is the amount of topical steroid that's squeezed out from the tube along an adult's fingertip (the distance from the tip of the adult index finger to the first crease) as shown in the image below.

Image credit: DermNet, NZ(external link)
- 1 FTU is enough cream or ointment to cover an area the same size as 2 adult handprints (palms and fingers).
- You'll need to use enough topical steroid to get a response, then you can use a less potent product to control the condition.
- If you’re using a topical steroid and not getting a response after 7 days, instead of using more or using it for a long time, talk to your healthcare provider. A short course of a stronger topical steroid can be safer than using a lower strength one for a long time.
- Your healthcare provider may ask you to cover treated areas. Covering the treated area after applying a topical steroid increases the absorption of the steroid but may also increase side effects.
-
If you have frequent skin flare-ups you may be advised by your healthcare provider to use treatment for a short time, to prevent flare-ups. This is also called ‘pulse dosing’ or ‘weekend treatment’ where you apply the topical steroid for 2 days a week during remission (between flares).
The diagram below gives some guidance on how many fingertip units of steroid cream are required for adults.
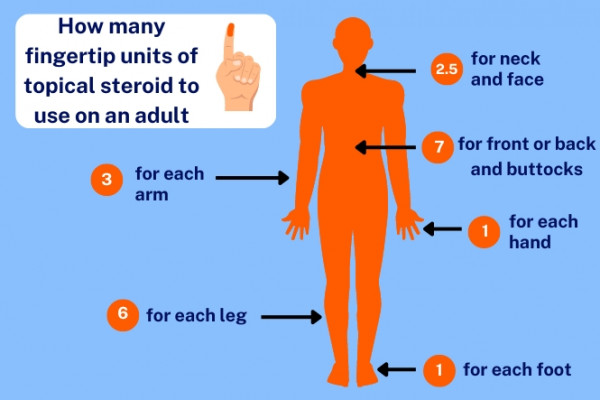
Image credit: Healthify He Puna Waiora
For guidance on how many fingertip units to use in children, read more about fingertip units when applying topical steroids to children(external link).
Video: How to use topical steroids
(Guy's and St Thomas' NHS Foundation Trust, UK, 2017)
Soak and smear method
If your topical steroid isn’t helping your skin condition, or if your symptoms are severe, you can try a method called ‘soak and smear’. Ask your healthcare provider if this method is suitable for you. Here is some guidance on how to do it:
- Have a lukewarm bath about 20 minutes before you go to bed. Gently pat your skin dry so it stays slightly damp.
- Smear a generous amount of topical steroid onto the affected areas.
- Wear loose-fitting clothes.
- In the morning, moisturise your skin.
If you find you need to use topical steroids every day for more than 2 weeks, or more than 3 times a week for most weeks, talk to your healthcare provider.
Like all medicines, betamethasone cream, ointment and lotion can cause side effects, although not everyone gets them. If you're worried about any symptoms, talk to your healthcare provider. The following information offers some guidance but doesn't include all possible side effects.
Tell your healthcare provider if these side effects bother you
- Burning or stinging feeling: This is common – talk to your healthcare provider if it's uncomfortable.
- Thinning of the skin: It can happen if a covering is used after treatment or if topical steroids are used often on a large area or long term. It's less likely to occur with mild or moderate topical steroids or if they're only used for a short course. If it does happen, it often goes away when the treatment is stopped.
- Permanent stretch marks, bruising, discolouration, thin spidery veins: These aren't common and may occur with long-term use of topical steroids.
Withdrawal side effects
If you use strong topical steroids every day for over a year and then suddenly stop using them, you may get a withdrawal reaction. The side effects of stopping treatment after a long time can include changes in skin colour, burning, stinging, itching or peeling skin. If you have been using topical steroids for a long time, talk to your healthcare provider about stopping treatment gradually to avoid these withdrawal side effects.
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
The following links provide further information on betamethasone:
Betamethasone (skin cream or ointment)(external link) New Zealand Formulary Patient Information
Betamethasone (scalp application)(external link) New Zealand Formulary Patient Information
Betamethasone (skin lotion)(external link) New Zealand Formulary Patient Information
Brochures
Identifying topical corticosteroids [JPG, 1.6 MB] Health New Zealand | Te Whatu Ora, NZ, 2025
Medicines and side effects [PDF, 91 KB] Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- Topical steroids(external link) New Zealand Formulary
- Betamethasone esters(external link) New Zealand Formulary
- Choosing a topical treatment for patients with chronic plaque psoriasis(external link) BPAC, NZ, 2017
- Topical corticosteroids for childhood eczema – clearing up the confusion(external link) BPAC, NZ, 2021
Brochures
Identifying topical corticosteroids
Health New Zealand | Te Whatu Ora, NZ, 2025
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland.
Last reviewed:





