- Low blood glucose or hypoglycaemia (sometimes called a hypo) is when your blood glucose level goes too low – for most people that's below 4 mmol/L.
- If you have diabetes (mate huka) and take insulin and/or sulphonylureas (glibenclamide, gliclazide, glipizide), you need to treat hypoglycaemia immediately to prevent going unconscious.
- Symptoms of hypoglycaemia include looking pale, feeling shaky, sweaty or unwell, sudden hunger, irritability, confusion and blurred vision.
- Treatment of hypoglycaemia for people with type 2 diabetes who weigh less than 70 kg, and for most people with type 1 diabetes, is to eat 15 g of a quick-acting carbohydrate (eg, 5 Mentos or 3 teaspoons of sugar mixed in water) immediately.
- People with type 2 diabetes who weigh over 70 kg should eat 30 g of rapid-acting carbohydrate (10 Mentos or 6 teaspoons of sugar mixed in water). These amounts may be less for children or people using an insulin pump.
- Retest your glucose level in 15 minutes, If it's above 4 mmol/L, have a carbohydrate snack (sandwich/crackers). If it's still below 4 mmol/L, repeat the same amount of rapid-acting carbohydrate and retest in 15 minutes.
- If you're getting hypos often (or have a sever hypo) then talk to your healthcare provider or diabetes specialist.
- If you don’t have diabetes or have diabetes but are not treated with insulin or sulphonylureas, a blood glucose level of 4 mmol/L is normal. If you feel shaky or very hungry, have a healthy snack or a meal if it is due. You are not at risk of becoming unconscious.
Low blood glucose
Also known as hypoglycaemia or a 'hypo'
Key points about low blood glucose (hypoglycaemia or a 'hypo')
- Low blood glucose or hypoglycaemia is when your blood glucose level goes too low – generally below 4 mmol/L.
- If you have diabetes (mate huka) and you're taking insulin and/or sulphonylureas you need treatment straight away as you may lose consciousness.
- You need quick-acting carbohydrate (eg, Mentos or sugar mixed in water) then retest your blood glucose level in 15 minutes.
- If it's above 4 mmol/L have a carbohydrate snack. If it's still below, have more quick-acting carbohydrate then test again in 15 minutes.
- Read more about how to recognise it and what to do below.

Symptoms of hypoglycaemia include:
- looking pale
- feeling shaky, sweaty or suddenly unwell
- suddenly feeling very hungry
- a 'racing' heart
- tingling around your mouth and tongue
- headache
- suddenly a little 'strange' as if you are unable to concentrate
- feeling dizzy
- rapid change in behaviour, or irritability
- confusion
- blurred vision.
If you have diabetes and think you're having a hypo, test your blood glucose level straight away, You are having a hypo if the reading is less than 4 mmol/L.
If you’re unable to test your blood glucose level and feel very unwell, treat your low blood glucose anyway. Always remember 'if in doubt, treat'. Hypoglycaemia needs to be treated right away to prevent the risk of unconsciousness.
Severe hypoglycaemia is a medical emergency. Call 111 and ask for an ambulance if someone has a blood glucose level less than 4 mmol/L and any one of the following:
|
Important: Do NOT try to give an unconscious person anything to eat or drink.
Continuous glucose monitoring (CGM)
If you're using a continuous glucose monitoring device (eg, Freestyle Libre, Dexcom), you should check your blood glucose level (eg, finger prick test) if:
- You have symptoms of low blood glucose but your sensor reads above 4 mmol/L: If your blood glucose level is below 4 mmol/L, you are having a hypo and must treat it immediately.
- Your sensor reads below 4 mmol/L but you don't have symptoms of low blood glucose: Only treat yourself for a hypo if your blood glucose level is below 4 mmol/L.
This is the recommended treatment for non-pregnant adults with diabetes
Step 1: Treatment for people with type 2 diabetes who weigh less than 70 kg and for most people with type 1 diabetes is to eat 15 g of a quick-acting carbohydrate (eg, 5 Mentos or 3 teaspoons of sugar mixed in water) immediately.
People with type 2 diabetes who weigh over 70 kg should eat 30 g (eg, 10 Mentos or 6 teaspoons of sugar mixed in water). These quantities may be less for children or people using an insulin pump.
If you feel very unwell, phone 111 for an ambulance.
Step 2: Retest your glucose level in 15 minutes. If it's above 4 mmol/L, go to step 3. If it's still below 4 mmol/L, eat another 15g (or 30 g) of carbohydrate, then retest in 15 minutes (steps 1 and 2). Keep repeating steps 1 and 2 until your blood glucose is above 4 mmol/L.
Step 3: Have a carbohydrate snack (sandwich/crackers) or a meal if it is due, then have a carbohydrate snack and retest your blood glucose again after 30 minutes to make sure it’s still at a safe level (over 4 mmol/L).
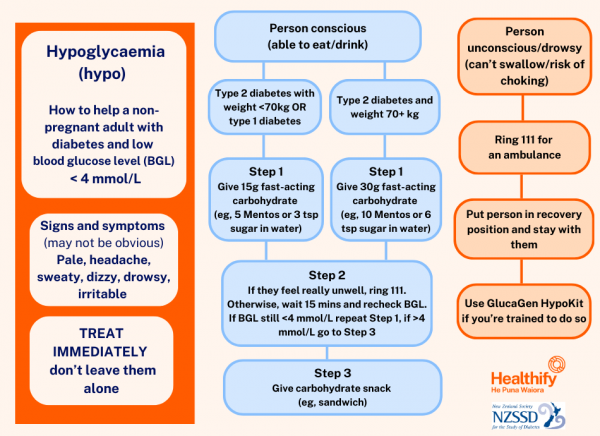
Image credit: Healthify He Puna Waiora and the New Zealand Society for the Study of Diabetes
How can I get 15 g of rapid-acting carbohydrate?
- 5 Dextro-Energy glucose tablets
- 4 Lift glucose tablets
- 15 g of glucose powder
- 3 teaspoons of sugar dissolved in water
- 150 mL (small glass) of fruit juice or non-diet soft drink
- 9 jellybeans
- 5 Mentos
- 1 tablespoon of honey
- 1 to 2 tablespoons of jam
- 1 Hypofit gel.
Double these quantities to get 30 g.
For the treatment of hypos in children, pregnant people or those using an insulin pump (particularly closed loop therapy), refer to the individualised instructions given to you by your diabetes care team.
Hypoglycaemia (a hypo) or low blood glucose occurs when your blood glucose level is less than 4 mmol/L, or where symptoms of hypoglycaemia are experienced at a level close to this.
Normally, when blood glucose lowers, your body lowers the amount of insulin it is putting out. This stabilises blood glucose by stopping glucose moving into your body’s cells and releasing stored glucose from your liver.
When you have diabetes and are taking insulin and/or sulphonylureas (glibenclamide, gliclazide, glipizide), you can still get the same low blood glucose level if you run out of glucose coming in from your food. But when your body senses that your blood glucose is becoming lower and it tries to switch off its insulin, it can’t. This is because you have injected your insulin (and you can’t switch this off).
This means the insulin continues to move glucose into your body’s cells and your liver doesn’t start releasing stored glucose. So, your blood glucose level keeps going down and can soon be dangerously low.
Your brain needs glucose all the time to function, so if you cut off the supply of glucose and don't take action, you'll eventually become unconscious.
Video: Hypoglycemia - What is hypoglycemia?
The following video from Diabetes UK helps explain the common symptoms, causes and treatment. This video may take a few moments to load.
(Diabetes UK, 2012)
Dangerously low blood glucose levels can occur in people with diabetes who are treated with insulin and/or sulphonylurea medication (glibenclamide, gliclazide, glipizide). The risk is higher for people who also:
- are older
- have had diabetes for a long time
- have had severe hypoglycaemia before
- eat irregular meals
- have reduced kidney function
- take beta-blocking medications (eg, metoprolol)
- drink a lot of alcohol.
The usual causes of a low blood glucose level are:
- an incorrect dose of insulin or sulphonylureas (talk to your diabetes care team if you think this needs to be adjusted)
- missing or delaying a meal
- missing snacks (if you need them)
- doing physical activity without either reducing your insulin or taking more carbohydrate before, during or after physical activity
- taking too much insulin
- drinking alcohol in excess or without eating carbohydrate food and/or reducing your insulin.
If you have type 1 or type 2 diabetes and you're often getting hypos, talk to your healthcare provider or diabetes specialist.
| If you have low blood glucose and you're feeling really unwell, call an ambulance. |
A serious low blood glucose level is classified as one you need the help of another person to treat. If the person is conscious and able to eat or drink, treatment is the same as above. Sometimes it can be easier to suck on a teaspoon of jam than chew glucose tablets. If a person has any difficulty swallowing, do not put any food in their mouth.
Call an ambulance if you find the person unconscious
If a person is unconscious from a hypoglycaemia episode, call an ambulance straight away. Place the person in the recovery position (lying on their left side with right leg hooked over the top of the left leg so they are leaning over, chin extended). If Glucagon is available and you know how to give it, then give right away. (Note that Glucagon takes 10 minutes to work.) Don't give an unconscious person anything by mouth as they may choke.
Glucagon injections
Glucagon is a naturally occurring hormone (also produced by your pancreas) that works in the opposite way to insulin. When blood glucose levels go too low, glucagon is released and this stimulates several processes to release glucose from your liver and fat stores into your bloodstream. However, injected Glucagon may need to be used as a treatment for serious hypoglycaemia. It comes as a GlucaGen HypoKit and can be given to someone with diabetes who is unconscious with a low blood glucose level.
Ask your diabetes specialist team whether a Glucagon injection is right for you. It can be a valuable addition to your emergency pack, especially if you do extreme sports or have little warning of hypos. It's also useful if you are a parent of a child with type 1 diabetes, whose eating and activity levels are harder to plan.
If you are given a Glucagon kit, make sure your whānau and friends are trained to know how and when to use it. This is what the kit looks like.
Read more about how to use the GlucaGen HypoKit [PDF, 274 KB].
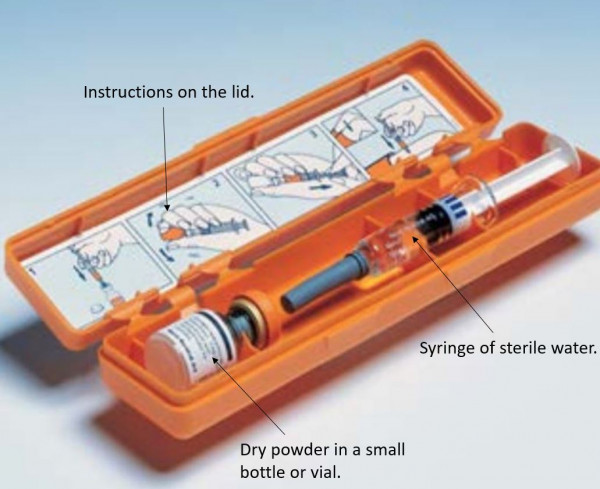
Image credit: Health New Zealand | Te Whatu Ora Waitematā
Wear identification
If you have type 1 diabetes or are on medicines that raise the risk of hypoglycaemia, wear a Medic Alert bracelet or necklace. Even with the best of care and planning, unexpected events can happen to trigger a serious hypoglycaemic episode. If this happens, an alert bracelet helps anyone helping you know what to do or to alert emergency services that you have diabetes if you are unable to ask for help. Without identification, there can be delays in receiving the right treatment.
Manage low blood glucose early
Learn to recognise your early warning signs of having a hypo. Be alert to what these are and test your blood glucose levels if any of these symptoms develop. Also make sure you always carry your emergency treatment (glucose/food) with you. Keep it in your bag, at work and at home so you can treat low blood glucose early before it becomes more serious.
Driving
If you take insulin or sulphonylurea medicines (glibenclamide, gliclazide, glipizide), always test your blood glucose level before driving. Legally, it must be 4.2 mmol/L or over to drive. “Above 5 to drive” is an easy way to remember.
If you have mild hypoglycaemia, the law states that you must not drive for 1 hour after that. If you have severe hypoglycaemia (when you need someone else's help to deal with it) and take insulin, you must not drive for 24 hours. If you take sulphonylureas, you must not drive for 48 hours.
People who experience severe hypoglycaemia while driving should not drive for at least a month, whether you're involved in a crash or not. Talk to your healthcare provider if this happens to you. It’s likely you’ll need to see a specialist before you can safely return to driving.
Read more about diabetes and driving.
Learn from a hypo
After any serious hypo, write down any possible triggers and what happened. Visit your diabetes specialist team to discuss what changes are needed to prevent further episodes.
Apps reviewed by Healthify
You may find it useful to look at some Diabetes apps.
If you have diabetes, you should already be in regular contact with your healthcare provider.
For people with diabetes taking insulin and/or sulphonylureas, you should also contact your healthcare team if:
- you're having frequent mild hypos
- you have had a serious hypo
- you're sick enough to not be able to eat as usual (you should also have a sick day management plan [PDF, 467 KB])
- you're planning a major change in your diet (keto diet, intermittent fasting, Ramadan)
- you have an upcoming procedure (eg, colonoscopy).
Please note that these links may not give the most up-to-date advice about the amount of glucose to take if you are having a hypo. This is because the New Zealand guidelines changed in mid-2023 and not all of these resources have been updated since then.
Hypoglycaemia in children with diabetes(external link) KidsHealth, NZ
What you need to know about hypoglycaemia(external link) Starship, NZ
Hypoglycaemia(external link) Diabetes Info NZ
Diabetes section(external link) Health NZ | Te Whatu Ora
Diabetes NZ(external link)
Apps
Resources
Diabetes and healthy food choices(external link) Diabetes NZ, 2019 English(external link), Chinese(external link), te reo Māori(external link)
Living well with diabetes Health New Zealand | Te Whatu Ora and HealthEd, NZ Cook Islands Māori(external link)
At home sick day plan [PDF, 467 KB] Health New Zealand | Te Whatu Ora
References
- Diabetes and driving(external link) NZSSD, NZ
- Management of hypoglycaemia(external link) NZSSD, NZ
Management of hypoglycaemia(external link) NZSSD
McTavish L, Corley B, Weatherall M, Wiltshire E, Krebs JD. Weight-based carbohydrate treatment of people with hypoglycaemia in people with type 1 diabetes using insulin pump therapy – a randomized crossover clinical trial(external link) Diabet Med. 2018;35(3):339-346.
Resources(external link) Aotearoa College of Diabetes Nurses
Diabetes and driving(external link) Waka Kotahi NZ Transport Agency
Apps
Brochures
HealthEd, NZ, 2019
Cook Islands Māori

At home sick day advice
Te Whatu Ora, NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Claire Salter, Pharmacist, Tauranga; Dr Ryan Paul, Endocrinologist, Hamilton
Last reviewed: