If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Tuberculosis
Also known as TB
Key points about tuberculosis
- Tuberculosis (TB) is a bacterial infection spread through coughing, sneezing or spitting.
- About a third of the world's population is likely to be infected with the TB bacteria. Most don't know they've been infected and have no symptoms (latent or sleeping TB).
- About 1 in 10 people with latent TB develop active TB at some point, often many years later.
- TB usually infects your lungs but can affect other parts of your body.
- TB can be very serious, particularly for young children and older people. It's treated with a combination of antibiotics for at least 6 months.
- If you've spent time with someone with active TB, see your healthcare provider.

Tuberculosis (TB) is an infection that's caused by a bacteria called Mycobacterium tuberculosis. The infection is spread through coughing, sneezing or spitting.
It's not common in Aotearoa New Zealand any more, but about a third of the world's population is infected with tuberculosis.
TB can stay inactive your body for many years before it develops. This is called latent tuberculosis infection. Even though you feel well and healthy, if you have latent TB your doctor may still advise treatment to make sure you don't develop active TB.
Active TB can cause serious lung damage, damage to other parts of the body it infects, and death.
Video: How the body reacts to tuberculosis
(Médecins Sans Frontières/Doctors Without Borders, UK, 2014)
Tuberculosis is spread from person to person through coughing, sneezing or spitting. The bacteria are carried into the air and people nearby can breathe them in through their mouths and noses.
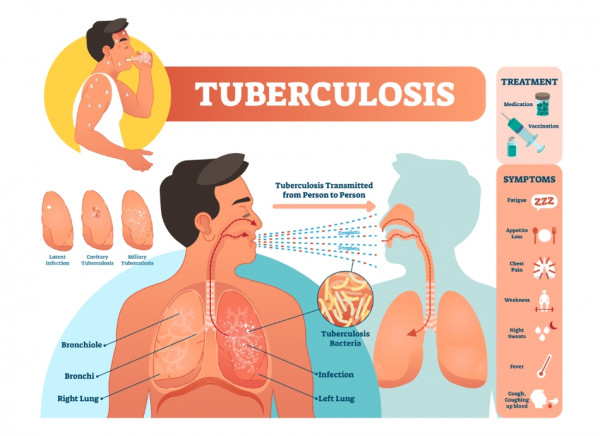
Image credit: Depositphotos
Some people are at greater risk of getting TB:
- People in close contact with someone who is a known case of active TB. Most children get TB from an infectious adult in their immediate or extended family/whānau.
- People living in institutions, including refugee camps and immigration centres, prisons, rest homes and mental health facilities.
- About 300 cases of TB are diagnosed each year in Aotearoa New Zealand. About half of these are in the Auckland region – 82% of these are new New Zealanders born in India, the Philippines or other countries in Asia. Of those born in Aotearoa New Zealand, over half are Māori.
- People regularly coming into contact with cows, deer, possums and certain animal products are at risk of getting bovine TB. This is very rare in Aotearoa New Zealand. The most likely source of exposure to bovine TB is drinking unpasteurised milk from an infected cow or handling an infected animal carcass.
You can't get TB from clothes, drinking glasses, eating utensils, toilets or other surfaces where a person with TB has been, or from shaking hands with them.
Most people who are infected with the TB bacteria don't have symptoms of infection, because the bacteria are not active. This is called latent (or sleeping) TB.
One in 10 people who have latent TB may develop active TB at some time in their lives. The risk of developing active disease is greatest in the first year after infection, but active disease often doesn't occur until many years later.
Can I catch TB from someone with latent TB?
A person with latent TB infection can't spread the bacteria to other people. You don't need to be tested if you have spent time with someone with latent TB infection. However, if you've spent time with someone with TB disease or someone with symptoms of TB, you should be tested.
How is latent TB diagnosed?
For some jobs in healthcare, or if you've been in contact with TB, you may be screened for latent TB. For most people this is a quantiferon gold (interferon gamma release assay) blood test. Children under the age of 2 need a tuberculin skin test (Mantoux test) which measures the skin reaction 2 to 3 days after they've had a small injection of purified tuberculosis protein into their skin. Read more about the Mantoux test(external link).
How is latent TB treated?
Not all people with latent TB are treated. Only people at high risk of developing active TB disease are treated, such as:
- people who have recently been exposed to TB disease
- people with certain ongoing medical conditions
- people taking certain medications that weaken their immune system.
Treatment for latent TB is antibiotics taken for 3 to 12 months. Treatment is effective in reducing your future risk of developing TB disease.
Symptoms of TB depend on which part of your body is affected. Tuberculosis of your lungs is by far the most common type.
Symptoms of TB in your lungs
- Ongoing cough (lasting 3 weeks or longer).
- Coughing up blood in your spit.
- Chest pain when you cough.
- Weight loss.
- Loss of appetite (not feeling like eating).
- Fever.
- Sweating at night.
- Feeling weak and tired.
- Feeling unwell.
- Swollen glands (usually in your neck).
If you have symptoms of TB or have been around someone who has TB, you should go to your healthcare provider for tests. To start with, you will usually have a chest X-ray to see if there is any active lung TB.
If the chest X-ray suggests that TB is possible, the next test is often to look for TB bacteria in your lung. This is done by sending samples of sputum (phlegm) to the laboratory. Other tests depend on where in your body your healthcare provider thinks your TB may be.
If you need treatment for TB you'll be referred to a hospital specialist. Your whānau will be checked for TB too.
TB is curable. However, the bacteria causing TB (Mycobacterium tuberculosis) can take a long time to get rid of.
Active TB (when there are symptoms) is treated with a combination of antibiotics for at least 6 months. A combination is used to prevent the bacteria becoming resistant. Examples of antibiotics used to treat TB include isoniazid, rifampicin, ethambutol and pyrazinamide.
- It is very important if you have TB to take your medicine regularly and finish the course of medicine.
- If you stop taking the antibiotics too soon, you can become sick again.
- If you don't take the antibiotics correctly, the bacteria that are still alive may become resistant to those antibiotics.
- TB that's resistant to antibiotics is harder and more expensive to treat.
- In some situations, healthcare providers meet with people who have TB to watch them take their medicines. This is called directly observed therapy (DOT).
- DOT helps you complete the treatment in the least amount of time.
If you have TB, there are a few things you can do to take care of yourself and protect your whānau and friends.
Take your medicine
Taking your medicine and finishing all of it is the best way to protect yourself and others from TB. If you stop your treatment early or miss doses, TB bacteria have a chance to develop mutations (changes) that allow them to survive even if you're taking TB medicine. These drug-resistant strains are much more difficult to treat.
Healthy eating and exercise
As well as taking your medicine, you can help your body fight the infection by eating healthy foods, and getting enough sleep and exercise. Many people lose weight because of the infection. If you're losing too much weight, eat balanced meals with enough protein and calories to help you keep weight on. Read more about how to put weight on.
Mental health and wellbeing
People often feel embarrassed about having TB and worry about other people finding out. It's also easy to feel isolated and alone because you can't go to work, school or public places until you can no longer infect other people. If you're feeling depressed or or down, tell your healthcare provider, or call or text 1737(external link) to talk to a counsellor for free any time day or night.
Reduce the spread
It usually takes a few weeks of treatment before you're not infectious (able to spread TB to other people). In the first 2 weeks, you can reduce the spread of infection by:
- staying home and not going to work or school
- avoiding sharing a room with others
- wearing a surgical mask when you are around others
- covering your mouth when you sneeze, cough or laugh
- airing or ventilating your room, because TB spreads more easily in closed spaces.
If you have latent TB (no symptoms), your doctor may advise you to take medicine to reduce your chance of getting active TB. By preventing latent TB from becoming active, you also won't spread TB to anyone else.
BCG vaccine
The BCG (Bacillus Calmette-Guérin) vaccine helps protect against severe forms of TB by helping your immune system fight against it. In Aotearoa New Zealand, the BCG vaccine isn't recommended for the general population because the rates of TB are quite low in many parts of the country.
BCG vaccination is recommended for babies or children under 5 years of age if they have a higher risk of getting TB. Read more about the BCG vaccine.
Tuberculosis (TB) HealthEd, NZ English(external link), Russian(external link), Ukraine(external link)
Tuberculosis(external link) Immunisation Advisory Centre, NZ
Tuberculosis disease(external link) Health New Zealand | Te Whatu Ora
Tuberculosis(external link) NHS, UK
Brochures
Brochures from other organisations that give you more information on tuberculosis, including in other languages.
Tuberculosis factsheet – Information about TB, including symptoms and treatment Health Ed, NZ English(external link), Russian(external link), Ukraine(external link)
BCG vaccine – information for parents(external link) HealthEd, NZ English(external link), te reo Māori(external link), Amharic(external link), Arabic(external link), Burmese(external link), Cambodian-Khmer(external link), Chinese (simplified)(external link), Chinese (traditional)(external link), Fijian(external link), Hindi(external link), Japanese(external link), Kiribati (Gilbertese)(external link), Korean(external link), Persian (Farsi)(external link), Pushto Afghani, Somali(external link), Tuvaluan(external link), Vietnamese(external link)
BCG vaccine – aftercare for parents(external link) Health Ed, NZ English(external link), te reo Māori(external link), Amharic(external link), Arabic(external link), Burmese(external link), Chinese traditional(external link), Chinese simplified(external link), Fijian(external link), Japanese(external link), Hindi(external link), Khmer (Cambodian)(external link), Persian (Farsi)(external link), Pushto(external link), Somali(external link), Vietnamese(external link)
Mantoux test(external link) Health Info Canterbury, NZ
Note: These resources are from overseas so some details may be different in New Zealand, eg, phone 111 for emergencies or, if it’s not an emergency, freephone Healthline 0800 611 116.
Tuberculosis factsheet(external link) NSW Multicultural Health Communication Service, Australia Samoan(external link), Tongan(external link), Chinese (traditional)(external link), Thai(external link), Vietnamese(external link)
Tuberculin skin test(external link) NSW Multicultural Health Communication Service, Australia English(external link), Samoan(external link), Tongan(external link), Chinese (traditional)(external link), Chinese (simplified)(external link), Thai(external link), Vietnamese(external link), other languages(external link)
What you should know about tuberculosis (TB)(external link) Association of Asian Pacific Community Health Organizations English(external link), Chinese(external link), Ilocano(external link), Korean(external link), Tagalog(external link), Thai(external link), Vietnamese(external link)
References
- Tuberculosis(external link) Immunisation Advisory Centre, NZ
- Guidelines for tuberculosis control in NZ(external link) Health New Zealand | Te Whatu Ora
- Antituberculosis drugs(external link) NZ Formulary
- BCG vaccine and vaccinator endorsement(external link) Health New Zealand | Te Whatu Ora
- Tuberculosis(external link) Auckland Region Community HealthPathways, NZ, 2024
Guidelines for tuberculosis control in NZ(external link) Health New Zealand | Te Whatu Ora
Tuberculosis treatment(external link) Starship Clinical Guidelines, NZ, 2017
The NZ laboratory schedule and test guidelines – microbiological and serological tests(external link) BPAC, NZ, 2014
Free health assessments for 2022 Special Ukraine Visa holders(external link) Health New Zealand | Te Whatu Ora, 2022
Free health checks for 2022 Special Ukraine Visa holders(external link) Health New Zealand | Te Whatu Ora, 2022
Public Health Unit contact details(external link) Health New Zealand | Te Whatu Ora
Brochures
Association of Asian Pacific Community Health Organizations (AAPCHO), 1995
Chinese, English, Ilocano, Korean, Tagalog, Thai, VietnameseCredits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed: