You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Rheumatoid arthritis | Mate rumatiki
Also known as RA
Key points about rheumatoid arthritis
- Rheumatoid arthritis (RA or mate rumatiki) is a chronic (long-term) inflammatory condition causing swelling, pain and stiffness in your joints.
- It can also affect other parts of your body.
- It can occur at any age, but most often appears between the ages of 25 and 50 years.
- RA is a common form of arthritis, affecting about 40,000 New Zealanders.
- It affects women more often than men, and smokers more than non-smokers.
- Early treatment can slow the progression of RA and can even lead to complete remission.

Rheumatoid arthritis (RA or mate rumatiki) is a long-term condition affecting your joints. Your body’s immune system attacks the lining of your joints causing pain, swelling and stiffness.
With continuous swelling and inflammation of your joints, the joint capsule remains stretched and can no longer hold the joint in its proper position. As a result, the joint may become unstable and this can lead to joint damage and deformity.
The image below shows a healthy joint and one that’s affected by rheumatoid arthritis.
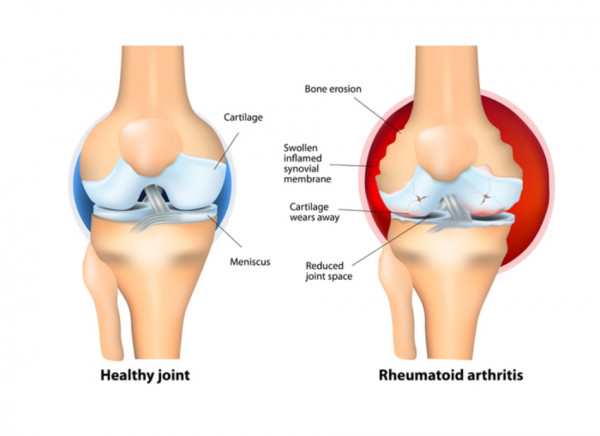
Image credit: National Library of Medicine, US, via Wikimedia Commons
Which joints are affected, and the extent to which they’re affected, varies a great deal from person to person. RA usually affects the small joints in your hands and feet, but it can affect many joints including your ankles, elbows, wrists, hips, knees, neck and shoulders.
The pain, stiffness, fatigue and whole-body (systemic) symptoms of RA can be severe and can mean you have difficulty with daily activities.
Effective treatment by a rheumatologist (a doctor who specialises in conditions affecting bones, joints, muscles, ligaments and tendons) can prevent joint damage and reduce other symptoms of RA. Getting treatment early can slow the progression of the condition, minimise joint damage and even lead to complete remission. Being in remission is a time when there’s very little disease activity and you may have very few or no symptoms. You may also have times when your symptoms get worse – these are called flare-ups or flares.
Rheumatoid arthritis usually starts quite slowly. The first things you might notice include:
- the joints of your fingers, wrists or the balls of your feet become uncomfortable or tender
- swelling in your joints, which often comes and goes
- joints are affected symmetrically – you’ll notice symptoms in the same joints on both sides of your body.
- feeling stiff when you wake up in the morning.
For some people, the disease develops very rapidly and there may be a sudden onset of pain and swelling in a lot of joints.
Flare-ups
Symptoms tend to come and go with no particular pattern. You may have periods of time when your joints become more inflamed and painful (flare-ups). Sometimes these flare-ups have an obvious cause (eg, physical injury, illness or emotional stress) but usually there’s no obvious cause. This can be frustrating and can make it difficult to plan ahead.
Other symptoms
Inflammation can also affect other organs, eg, your eyes (causing dry, irritable, red and painful eyes), lungs (causing difficulty breathing), heart and kidneys, skin, nerves, and blood vessels.
Rheumatoid nodules (fleshy lumps) may sometimes appear, usually just below your elbows, but they can also occur on your hands and feet. Anaemia (low red blood cell count) is common. Occasionally this can be a side effect of the drugs used to treat RA, but it’s more often caused by the disease itself.
Long-term impact
Long-term, rheumatoid arthritis affects people differently:
- rarely, it lasts only a year or two and goes away without causing any noticeable damage.
- Other people have mild or moderate forms of the disease, with periods of worsening symptoms (flare-ups) and periods in which they feel better (remissions).
- For some people, ongoing inflammation can increase their chance of joint damage and other problems, eg, heart disease.
Video: Rheumatoid arthritis
(NHS Choices, UK, 2020)
RA is an autoimmune disease, which means your body's defence system (your immune system) is confused and attacks its own cells that line the inside surface of joints. The exact cause isn't fully understood.
- Genes that you inherit from your parents don’t cause RA but may play a role. This can increase your chance of developing RA.
- Women are affected 3 times more often than men.
- Smokers are more likely to develop RA than non-smokers. Smoking can increase the chances of developing RA by 40 times. It may also worsen joint damage and contribute to osteoporosis (thinning of the bones).
- Some people find that cold, damp conditions and changes in the weather can affect their symptoms, but there’s no evidence that the weather causes rheumatoid arthritis or affects its progression.
If you have painful or swollen joints, see your healthcare provider. Early diagnosis is important as treatment does help and reduces long-term damage to your joints.
There’s no single test that can result in a certain diagnosis of early RA. Health professionals have to make a clinical diagnosis, based on discussion with you, a physical examination and the results of laboratory tests and sometimes X-rays.
Tests
Your healthcare provider may suggest any of the following tests and investigations.
- Full blood count: This test measures how many of each type of blood cell are in your blood. This may show anaemia as well as abnormalities in white blood cell counts or platelet counts that could be associated with RA.
- Inflammation markers: C-reactive protein (CRP) levels may be high in RA, but not always.
- Immunologic tests: Levels of rheumatoid factor (RF) and other antibodies (anti-CCP) may be checked. About 80% of people have a positive RF.
- X-rays and other imaging techniques: X-rays can reveal damage caused to the joints by RA. Magnetic resonance imaging (MRI) and ultrasound scanning may also be used. They are more sensitive in picking up changes and are being studied to see how useful they are for diagnosing early disease and for monitoring its progress.
Starting treatment as soon as possible after a diagnosis has been made can help prevent permanent joint damage.
Although there's currently no cure for RA, a variety of treatments are available that can slow down the disease and reduce the damage to your joints and other parts of your body.
A combination of both medicines and non-medicine approaches are best. Medicines may include non-steroidal anti-inflammatory drugs (NSAIDS), steroids, disease modifying drugs (DMARDS) and biological therapies (biologics). Read more about the medicines used to treat RA.
Non-medication approaches
- If you are a smoker, stop smoking as there's evidence that continuing smoking can make it less likely that RA medicines will work well for you.
- Physiotherapy helps preserve and improve your range of joint motion, increase your muscle strength, and reduce your pain.
- Hydrotherapy involves exercising and relaxing in warm water. Being in water reduces the weight on your joints. The warmth relaxes your muscles and helps relieve pain.
- Occupational therapy teaches you ways to use your body efficiently to reduce stress on your joints.
- Self-management skills learned through arthritis educator clinics, seminars and self-management programmes will give you the tools and techniques you need to self-manage your RA.
- Surgery is occasionally needed. Operations vary from quite minor ones (eg, the release of a nerve or a tendon) to major surgery (eg, joint replacement).
- Regular medical check-ups are an important part of managing RA. These include checking blood pressure and monitoring cholesterol and other risk factors for heart disease.
Lifestyle measures are an important part of self-management in RA.
- Take care of your joints by finding a balance between rest and physical activity – rest may make your inflamed joints comfortable, but without movement your joints will stiffen and your muscles will weaken.
- Exercise is a very important part of a complete treatment plan for RA. It helps reduce your pain and fatigue, increases your range of joint motion and strength, and keeps you feeling better overall. Talk to your physiotherapist about the most appropriate exercise regime for you. Read more about exercising with arthritis(external link).
- Make your working life easier by finding ways to achieve what you need to do while managing your pain and tiredness and reducing the strain on your joints. The key to success is to do a variety of tasks, in stages, and with rest breaks. Occupational therapists may have lots of helpful tips for how to do this.
- Both heat and cold treatments can relieve pain and reduce inflammation. Some people find their pain responds better to heat whereas others find it responds to cold.
- Relaxation techniques are beneficial for releasing muscle tension, which helps relieve pain.
- Live a healthy life. Stay physically active, eat a healthy diet, stop smoking and reduce stress to help your overall health and wellbeing.
- Ask your doctor about fish oil, some studies have demonstrated beneficial effects of fish oil supplementation in decreasing pain.
Apps reviewed by Healthify
You may find an app useful to help you learn more about rheumatoid arthritis and manage it better. Healthify has reviewed some apps for people with arthritis.
Being a good self-manager is important for living well with RA. This doesn’t mean you have to manage entirely on your own. Instead it means that you work together with your healthcare provider (and whānau and friends) to manage your condition, improve your health and enjoy a better quality of life.
Here are some things that can help you live well with RA.
Adjust your routine
Joint swelling and pain can make it difficult to complete daily tasks – things you used to do with ease, may be more challenging.
Understanding your limitations and making small adjustments to your daily routines may make things easier. This may include doing your tasks in stages with rest breaks and re-organising your environments (eg, your kitchen or work space) so that items you use frequently are easy to reach.
Make your home life easier
There are ways you can make tasks around the home easier if you have RA. For example:
- slide objects along a bench rather than lifting them
- use carts or trolleys to transport large or heavy items
- use reach-extending tools to get hard-to-reach items
- use both hands to pick up objects whenever you can
- use specialised tools or equipment to make the job easier eg, a jar opener to get lids off jars, long-handled shoe horns for putting on shoes
- organise workspaces so that items you use the most are within easy reach
- don’t rush when doing housework and take regular breaks.
You can ask to see an occupational therapist (OT) for advice. An OT is a health professional who can give you advice on how you can take stress and strain off your joints. They will look at the things you do at home (or at work) and can show you how to simplify tasks to protect your joints. They can also recommend any special equipment that will help make daily tasks easier.
Understand your medicines
- Get the most out of your medicines by taking them regularly, as prescribed.
- Even if you feel better, taking your medicine can help prevent flare-ups and reduce the risk of joint damage. See our tips for remembering to take your medicines.
- Also, get to know your medicines, their side effects and what to do if they occur, anything you can do to lessen side effects, and any tests or monitoring that may be needed. By having a better understanding of your medicines, you have a greater chance of taking them properly and safely.
- Arthritis medicines may interact with over-the-counter medicines or herbal supplements, so check with your healthcare team or pharmacist before using these.
Make healthy lifestyle choices
Maintaining a healthy lifestyle will help your physical and mental wellbeing.
Doing gentle, regular exercises(external link) can help keep your joints flexible, strengthen your bones, help you maintain a healthy weight, relieve emotional stress and create a feeling of general wellbeing.
Eat a well-balanced diet with a high intake of whole grains, vegetables, fruits, legumes, nuts, fish and olive oil. There’s no specific diet for people with RA and no specific foods to avoid.
Vaccination advice
People with RA are at increased risk of infection, so it’s important that all your vaccinations (eg, influenza, Covid) are up to date. Talk to your healthcare team about making sure you get the vaccines you need.
Have a support network
Adjusting to life with RA can be challenging and frustrating. It can be hard to deal with the unpredictable nature of the condition. Some days, the pain and stiffness will be much worse than others, and there's no way of knowing when a flare-up will occur.
You may feel angry, anxious, sad, discouraged and depressed. This is normal.
Many people find it helpful to talk to others in a similar position. You may find support from an individual or group of people with rheumatoid arthritis. Arthritis NZ has online support groups(external link) moderated by a health advisor.
Talk to your healthcare team if you're struggling emotionally and your low mood is affecting your daily activities.
Plan for setbacks
Many people with RA find that they can achieve remission with either a total absence of symptoms or having only an occasional flare-up of joint symptoms or morning stiffness. But flare-ups may occur and it's not unusual to alternate between periods of flares (relapse) and being free of symptoms.
These periods of relapse can be difficult to deal with. Symptoms you once had under control, can return.
Understanding why relapses occur and planning for setbacks can help you manage them better.
Talk to your healthcare provider about how to manage flare-ups and know who to contact for help or advice when you need it. Make plan for how you'll manage tasks at home and work during a flare-up.
Have your say – shared decision making
Talk to your healthcare provider about any part of your care that you’re not satisfied with. Together you can find solutions or the support you need.
While your healthcare team may have expert knowledge in the diagnosis and treatment of your condition, remember you have the best understanding of how you're feeling, what your expectations are, and what things are important to you. Therefore, together you and your team can find the best choices for you.
Here are some examples of questions to ask your rheumatologist (specialist):
- How will I know if my medicine is working, and how long does this take?
- What are the possible side effects and how often will they occur?
- What should I do to minimise the chance of side effects?
- Who do I contact if I have concerns about the medicine?
- Are there medicines I should stop now that I’m beginning this new treatment?
- How can I keep track of the blood test results used to monitor my RA?
Apps reviewed by Healthify
You may find it useful to look at some Physiotherapy and exercise apps and Arthritis apps.
Social events and meeting people with similar problems may help you to deal with day-to-day activities and provide emotional support. Arthritis NZ(external link) provides a range of services to all New Zealanders affected by arthritis.
Aids and accessories for making it easier to live with RA can be found at the Mobility Centre(external link) or at Independent Living Charitable Trust(external link).
Rheumatoid arthritis(external link) Arthritis NZ
Rheumatoid arthritis(external link) Rheumatoid Arthritis Support Network, US
Taking control of your rheumatoid arthritis(external link) Arthritis Australia
At home with arthritis – simple steps for managing in the home(external link) Arthritis Australia
Brochures
What is rheumatoid arthritis? (RA)(external link) Factsheet Arthritis NZ
Rheumatoid arthritis(external link) Arthritis NZ, 2025
In the kitchen with arthritis(external link) Arthritis NZ
Arthritis – exercises to keep you moving(external link) Arthritis NZ
Rheumatoid arthritis – Arthritis information sheet(external link) Arthritis Australia. Also available in Assyrian(external link), Mandarin(external link), Korean(external link), Spanish(external link), Punjabi(external link), Arabic(external link), Chinese(external link), Greek(external link), Italian(external link), Vietnamese(external link)
Arthritis NZ provides factsheets(external link) on a wide range of topics including:
- managing flare-ups
- tips for arthritis in your hands and feet
- the effect of diet on arthritis
- healthy activity and arthritis
- getting the most out of your appointments
- a wellbeing toolbox.
Apps/tools
Arthritis tools
Physiotherapy and exercise apps
Arthritis apps
References
- Biologic medicines for the treatment of inflammatory conditions – what does primary care need to know?(external link) BPAC, NZ, 2013
- Rheumatoid arthritis(external link) Mayo Clinic, US, 2023
- Rheumatoid arthritis in adults – management(external link) NICE, UK, 2020
- Frankel L, Bathon JM, England BR, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis(external link) Arthrit Care Res. 2021;73(7):924-939
- At home with arthritis – simple steps for managing in the home(external link) Arthritis Australia, 2019
- Rheumatoid arthritis consumer care guide(external link) Arthritis Australia, 2024
- In the kitchen with arthritis(external link) Arthritis NZ
Rheumatoid Arthritis – monitoring of DMARDs (external link) BPAC, NZ, 2008
Cochrane Reviews of Arthritis Treatments(external link) Cochrane Library
PHARMAC seminar; Rheumatology update 1 of 5, Rheumatoid arthritis – Assoc. Prof. Andrew Harrison (36 minutes)
(PHARMAC, NZ, 2018)
For more videos in the same series, view Rheumatology update(external link).
Apps/tools
Arthritis tools
Physiotherapy and exercise apps
Joint and bone health apps
Brochures

Arthritis NZ, 2025

Arthritis NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:






